OIP Hosts Carlisle Chamber Mixer
On Thursday April 25th, OIP was proud to host the annual Carlisle Chamber Mixer at our popular Carlisle office! With more than 70 people in attendance it was a huge success!




Mako Robot – Your Possible Answer to Knee Joint Replacement
OIP is Now Seeing Pediatrics!


PA Orthopaedic Society: Medical liability Venue Shopping Would Hike Costs, Threaten Care
Feb. 4 news conference proposes blocking legislation
The possible return of medical liability venue shopping, in a proposal now moving behind the scenes
at the Pennsylvania Supreme Court, threatens to plunge Pennsylvania into a crisis that could drive up
health insurance premiums while forcing medical professionals to leave the state.
State lawmakers will join the Pennsylvania Orthopaedic Society at a Capitol news conference on Feb. 4
to discuss legislation meant to stop the change.
Since 2002, Pennsylvania courts have not allowed medical liability “venue shopping” – the ability by
plaintiffs to file suit in favorable courts, regardless of where an incident occurred. The rule, supported
by lawmakers and then-Gov. Schweiker, ended a crisis that had been gripping the health care
community since the late 1990s. In the ensuing 17 years, Pennsylvania’s medical liability system has
operated under this common-sense rule, said POS President Asif Ilyas, MD.
Under a new venue rule proposed on Dec. 22, 2018, the Supreme Court’s Civil Procedural Rules
Committee recommended that plaintiffs have broadly expanded powers to file lawsuits far from the
site of any alleged malpractice. While the current rule restricts proceedings to the county of
occurrence, the change would allow filings in counties that fit such locational criteria as where
defendants live, related procedures were conducted, or suppliers, health networks, and investors
have offices.
“This change is unwise and misguided,” said Dr. Ilyas. “Twelve million Pennsylvanians rely on their
medical professionals for care that delivers the best possible quality of life. As we know from past
experience, venue shopping opens the floodgates to a deluge of unjustifiable lawsuits, filed in places
with only specious connections to the cases. If Pennsylvanians wanted this rule change, they would
have spoken up years ago. They don’t want to see higher health costs. They don’t want to stand by
helplessly as their trusted physicians are forced to close their doors as happened in the early 2000s.”
The Supreme Court is taking public comment on the proposed changes to Pennsylvania Rule of Civil
Procedure 1006 through Feb. 22.
“Please visit “
www.PAGOPpolicy.com to voice your opinion, before 2/22/2019, on
https://pcntv.com/2019/01/31/m
View PCN COVERAGE of the February 4 press event.
|
Treatment Options for Carpal Tunnel and Wrist Pain
Are you noticing a numb, weak, pins-and-needles or falling asleep sensation in your hand and wrist? What about pain in your wrist? Perhaps, all of these sensations are occurring for no apparent reason. If you’re having these symptoms, chances are you could be experiencing carpal tunnel syndrome.
It’s best not to delay carpal tunnel treatment or wrist pain treatment, as ignoring the symptoms of this common condition could lead to permanent nerve damage. If you suspect you have carpal tunnel syndrome (CTS), visit us at the Orthopedic Institute of Pennsylvania (OIP) to receive an official diagnosis and begin treatment.
What Is Carpal Tunnel Syndrome?

Carpal tunnel syndrome is a relatively common condition affecting your wrist and hand. It’s estimated to affect up to 6 percent of people in the U.S., particularly in the 45 to 64 age group. Since the narrow passageway on the palm side of the wrist, known as the carpal tunnel, is often smaller in women than men, women are three times more predisposed to the condition than their male counterparts.
Your symptoms may begin in a mild form initially, but as the condition progresses, you can find CTS becomes more bothersome and painful. You may first notice numbness or tingling in your fingers off and on. But, the sensations can become worse over time, last longer and even wake you up at night. Eventually, the numbness and pain could make it difficult to grips things like a pen, fork or another object.
This condition occurs when your median nerve — the nerve passing through the carpal tunnel, or narrow space that runs to your hand from your forearm — is pinched or compressed. The median nerve controls the movement and sensations in the pointer, middle and ring fingers, as well as the thumb. You usually experience it in your dominant hand first, which is typically where you will feel the most severe pain.
Risk Factors for Carpal Tunnel Syndrome

Anything that makes your carpal tunnel smaller, pinching the median nerve, may lead to carpal tunnel syndrome. These may include:
- Repetitive Hand Movements: Although repetitive activities like typing on the keyboard were thought to induce carpal tunnel syndrome, research now shows this isn’t the most prominent cause. Regular use of vibrating or heavy equipment, such as a jackhammer, can predispose you to carpal tunnel syndrome. You’re also more likely to develop CTS if you regularly bend your wrist at a higher level than your hands.
- Medical Conditions: Certain medical conditions can cause carpal tunnel syndrome, such as rheumatoid arthritis, hypothyroidism and diabetes. For instance, people who have diabetes and other metabolic disorders that affect the nerves of the body are more vulnerable to compression, so they have a higher risk of developing CTS, according to the National Institute of Neurological Disorders and Stroke (NINDS). Children do not usually experience carpal tunnel syndrome.
- Pregnancy: If you have edema, or a build-up of fluid in your wrist tissues during pregnancy, you can develop carpal tunnel syndrome. CTS typically disappears shortly after giving birth.
- Occupation: The chances of developing carpal tunnel syndrome aren’t confined to individuals in a single job or industry, but it’s particularly common in people who perform assembly line work like cleaning, packing or manufacturing. In fact, assemblers are three times more likely to develop carpal tunnel syndrome than data entry personnel.
Treatment Options for Carpal Tunnel and Wrist Pain

Here are nine potential treatment options for carpal tunnel — although it’s always smart to see a doctor to determine the best method for you.
1. Wear Splints or Braces
You can help relieve median nerve pressure by keeping your wrists straight. Individuals often experience symptoms more at night. If this is the case for you, wearing a splint during the evening can help alleviate your symptoms before they begin. You may also wear a splint brace during the day if you have problems at work with repetitive tasks.
Braces are typically best when you’re experiencing mild to moderate symptoms of carpal tunnel syndrome. While they might not work for everyone, it doesn’t hurt to try one since no adverse side effects are involved. Give it a few weeks to see if your symptoms improve.
The doctor will likely recommend you wear a brace during the night when you’re in bed. This is because many individuals bend their wrists while sleeping and this can worsen the symptoms.
2. Take Medications
Several types of medications serve as treatment options for wrist pain, including:
- Over-the-Counter (OTC) Medications: In some cases, drugs can help ease the swelling and pain linked with carpal tunnel syndrome. For instance, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin might offer you short-term relief from pain and discomfort, but they don’t treat the condition.
- Topicals: One study showed slaughterhouse workers with carpal tunnel syndrome who applied topical menthol during the workday significantly reduced their pain. If you would like to try a topical, consult with your doctor and be sure to follow the directions on the package.
3. Ice Your Wrists
Soak or ice your wrist in an ice bath for around 15 minutes once or a couple of times an hour. Icing may help relieve the pain.
4. Perform Wrist Exercises and Therapy
Here are a few wrist exercises you can try to relieve pain:
- Shake It Out: Once an hour for one or two minutes, shake your hands as if you’re trying to air dry them after washing them. By doing this, you’re helping to keep your hand flexor muscles and the median nerve from becoming tight and cramped during the day. You may already be doing this just by washing your hands frequently throughout the day.
- Wrist Flex and Extend: For this exercise, you’ll hold your arm in front of you straight out, keeping your hand and wrist straight and palm facing down. Start bending your wrist down, so you’re pointing your fingers toward the floor. Using your other hand, start pulling your fingers gently toward your body to help increase the stretch. Hold this position for up to 30 seconds. Now, return to a neutral, straight wrist position with palm still facing down. Begin bending your wrist up, so you’re pointing your fingertips toward the ceiling. Gently pull your fingers with the other hand back toward you, holding the position for another 30 seconds. Repeat 10 times a few times a day.
- Stretch It Out: Whether you’re sitting at your desk or standing in line at your local grocery store, you can perform this simple and quick wrist exercise. Make a fist and release, so your fingers are straight again. Continue performing this exercise up to 10 times to help relieve any pressure you may have in your wrist.
5. Change Your Activities
Often, carpal tunnel syndrome will flare up when you have been holding your wrist and hand in the same position for a long time. Keeping your wrist bent up or down can make it even worse — therefore, you should try to maintain a neutral, straight position the best you can. If your work makes this difficult, you might want to:
- Lighten Up: If you’re finding you are forcing or straining with tasks like typing or writing, reduce the force you’re using or relax your grip. Try tapping the keys a little lighter or use a soft-grip pen.
- Take a Break From Repetitive Tasks: Whether you’re using a hand drill, playing a guitar or typing, set a timer for 15 minutes before you start. Once it goes off, it’s time to take a break and wiggle your fingers. Move your wrists and stretch your hands to improve blood flow in these areas.
- Be Aware of Your Flexion: Avoid performing activities that cause you to flex your wrists in either direction to the extreme. Try to keep your wrists in a neutral position as much as you can.
- Keep Your Hands Warm: You can ease stiffness and pain by keeping your hands warm. Consider keeping hand warmers close or wearing fingerless gloves. Or, soak your hand in water that’s between 92 and 100 degrees, gently flexing your wrist and moving your hand. Repeat this several times a day.
- Use Only as Much Force as Required: Don’t pound away on your keyboard or hold your tools too tightly.
- Elevate Your Wrists and Hands Whenever You Can: This could be especially beneficial if fractures, pregnancy or fluid retention caused your carpal tunnel syndrome.
- Improve Your Posture: Don’t roll your shoulders forward, as this can set off a chain reaction and worsen the problems with your wrist.
6. Start Physical Therapy
A physical or occupational therapist can help in several ways. They might provide you with exercises for stretching and strengthening your wrist and hand muscles. They may also show you how to make changes to your regular motions in a way that eases the stress from your wrists and hands. These exercises could be particularly helpful when you’re performing activities related to your favorite hobbies or work.
7. Consider Alternative Therapy
Incorporate alternative therapies into your plan to help you manage your carpal tunnel syndrome. You may need to experiment with a few options to determine which treatment will work best for you. Always consult with your doctor before you try any alternative or complementary therapy.
As you try to figure out how to relieve wrist pain, you can test out these alternative therapies:
- Yoga: Yoga postures intended for stretching, strengthening and balancing your joints and upper body can help you decrease your pain and improve your grip strength.
- Acupuncture: Acupuncture is an excellent solution for many because it is low-risk and minimally invasive. In one study published in the journal Brain, researchers concluded that acupuncture helped to relieve pain for individuals with carpal tunnel syndrome. According to the researchers, the acupuncture “remapped” the brain, helping to reduce symptoms. They also said acupuncture provides direct healing effects to the source of the pain in the individual’s wrists. High-tech imaging showed acupuncture led to some mapping changes in the brain. Additionally, participants seemed to experience some healing effects in their wrists.
- Hand Therapy: Research shows certain occupational and physical hand therapy methods could reduce carpal tunnel syndrome symptoms.
- Ultrasound Therapy: High-intensity ultrasounds may help to raise the targeted body tissue area’s temperature to decrease pain and encourage healing. The research found varying results with this treatment, but an ultrasound therapy course over a few weeks could help decrease symptoms.
8. Discuss Steroid Injections With a Physician
Your physician might provide a corticosteroid, like a cortisone injection, to your carpal tunnel to relieve pain. In some cases, your doctor might use ultrasound for guiding these injections. Corticosteroids reduce swelling and inflammation, helping to relieve pressure on your median nerve.
9. Talk to a Doctor About Surgery
Typically, surgery will involve severing a ligament around your wrist to help reduce median nerve pressure. Surgery is generally performed under regional — involving some sedation — or local anesthesia and doesn’t require an overnight stay at the hospital. Many individuals need surgery on both hands.
Although carpal tunnel surgery involves the surgeon relieving nerve pressure by cutting the ligament, they can use two different methods to accomplish this:
- Open Release Surgery: Open release surgery is the standard surgery used for correcting carpal tunnel syndrome. The surgeon makes a two-inch incision in your wrist and cuts the carpal ligament so they can enlarge the carpal tunnel. Usually, patients require local anesthesia for this surgery, and it’s performed on an outpatient basis.
- Endoscopic Surgery: Endoscopic surgery may allow for less post-operative discomfort and quicker functional recovery than the standard open release surgery. There could, however, be more complications, and you may require additional surgery. The surgeon will make an incision — or two — of around a half an inch in your palm and wrist. Then, they’ll insert a camera which is attached to a tube so they can observe the ligament, nerve and tendons while cutting the carpal ligament.
After surgery, the ligaments will typically grow back together, allowing more space than before. While surgery may help relieve symptoms immediately after the procedure, full recovery can take several months. Usually, patients notice a decrease in their grip strength, but this improves over time. Some people might develop nerve damage, infections, pain and stiffness at the scar.
Call Orthopedic Institute of Pennsylvania to Set Up Your Carpal Tunnel and Wrist Pain Appointment

Carpal tunnel syndrome can be disruptive to your everyday life and painful. If you’re experiencing carpal tunnel syndrome symptoms, make an appointment with a doctor to receive an official diagnosis and relieve the pressure and pain you’re experiencing. Receiving an early diagnosis and treatment can help you prevent permanent nerve damage.
Orthopedic Institute of Pennsylvania is based in central Pennsylvania and committed to providing quality care and treatment to our patients. Contact us whether you recently started experiencing pain or have been for some time. We can provide you with holistic treatment options to help you get back to your pain-free life.
Most of our providers are specialists who can provide you with specialized care. We offer numerous treatments and services and are pleased to say 95 percent of our patients didn’t require orthopedic surgery to alleviate their problems. Schedule an appointment at any one of our eight locations to start treating your carpal tunnel syndrome today.
Chronic Back Pain Treatment Options – What’s Best For You?
If you are struggling with back pain in Central Pennsylvania, you’re part of a vast group. Around 80 percent of adults, at some point in their lives, experience back pain. It’s one of the most common contributors to missed work days and job-related disability, according to the National Institute of Neurological Disorders and Stroke (NINDS). The Orthopedic Institute of Pennsylvania (OIP) provides chronic pain treatment options at our eight locations, including conservative methods and surgical procedures if needed.
About Chronic Back Pain

Most lower back pain is short-term — or acute, lasting for several days to several weeks. But, it often resolves on its own with no residual function loss. Most acute back pain is mechanical, which means there’s a disturbance in how the back’s components — muscle, spine, nerves and intervertebral discs — fit together and move.
Chronic back pain, on the other hand, persists for over 12 weeks even if doctors treat an underlying cause or injury. Around 20 percent of individuals with lower back pain end up developing chronic low back pain with symptoms that persist for at least one year.
If you’ve been suffering from chronic back pain, it’s important you visit us at the OIP to receive a diagnosis for your condition and start treatment to experience pain relief.
Chronic Back Pain Treatment Options
Some treatment options for back pain and lower back pain include:
1. Medications
There are various categories of medicines used for treating chronic pain. Generally, your doctor, pharmacist or pain management specialist can answer your questions regarding the dose and side effects of these medicines. Here are some common medications used for treating chronic pain:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): There are some NSAIDs (like ibuprofen) you can obtain over-the-counter (OTC). NSAIDs could be effective for acute bone and muscle pain along with some forms of chronic pain conditions — like chronic back pain.
- Acetaminophen: You can also easily obtain acetaminophen over-the-counter, but you don’t want to take more than directed because it can have effects on your liver if you take too much. Many opioid medications have acetaminophen in them.
- Antidepressants: Some antidepressants can be helpful in controlling back pain, particularly the tricyclic antidepressants. These medications often relieve pain in lower doses than the standard doses required for treating depression. You don’t take these medications on an “as needed” basis since you have to take them every day regardless of whether or not you’re experiencing pain.
- Muscle relaxants: These drugs are used most often with acute muscle spasms. They are effective at relieving back pain.
- Opioids: Opioids are prescription medications that can effectively control different types of pain when used appropriately. They often require a higher dose with nerve type pain because a normal dose isn’t as effective. Your doctor will prescribe the right amount. For nerve type pain, a doctor might prescribe a long-acting opioid medication. Opioids have an addiction risk, so physicians don’t routinely prescribe them as a first option.
2. Injections
Epidural steroid injections, nerve ablations, nerve blocks and other forms of injection-based procedures can help with chronic back pain relief. Physicians may use them when they don’t know the cause of your pain. They also can sometimes help rule out specific causes if your treatment isn’t working. Injections might lessen or stop the pain for a certain period, but they’re not intended to provide you with a long-term solution, and you shouldn’t use them on their own.
Some common chronic back pain injection procedures are:
Epidural Injections
Epidural steroid injections are one option used for delivering pain medication quickly into your body using a syringe. The doctor injects the medication into the epidural area. This area covers your spinal cord, protecting it and your surrounding nerves from damage.
With an epidural steroid injection, your doctor will use an X-ray machine to guide the needle as they make the injection to ensure the needle is in the right area.
Radiofrequency Ablation (or RFA)
An RFA is a procedure doctors use to reduce pain. RFA is an effective and safe chronic back pain treatment option that’s typically well-tolerated, with barely any associated complications. There’s a very small risk of bleeding and infection at the site of insertion.
The doctor may place an intravenous (IV) line in a vein in your arm before the procedure to deliver a mild sedative and local anesthetic to reduce any discomfort during your RFA procedure. With the local anesthesia, you’ll still be awake, but you won’t feel any pain.
The doctor inserts a small needle into the area you’re experiencing pain. They use an X-ray machine, like with an epidural injection, to guide the needle to the precise area. They then insert a microelectrode through the needle and start the stimulation process. You may feel a tingling sensation.
Before the procedure, you may receive an intravenous (IV) line through vein located in your arm and a mild sedative or local anesthetic to reduce any discomfort during RFA. You may be awake during the process to aid in properly assessing the procedure. Ask your doctor about specifics beforehand.
The doctor places an electrode and needle to send a small radiofrequency current into the surrounding tissue through the electrode, heating the tissue.
Nerve Blocks
Nerve blocks are procedures used for managing or preventing different types of pain. They’re often injections of medications intended for blocking pain from certain nerves. They’re good for pain relief, too.
Nerve blocks use needles, usually combined with ultrasound, fluoroscopy — a tool with a fluorescent screen doctors use to view X-ray images — or CT scan or guide the needle correctly. The doctor might also use low-level electrical stimulation for locating which nerve is causing your pain.
3. Physical Therapy
The best treatment for chronic lower and upper back pain is physical therapy. Doctors tend to prescribe this type of treatment first. You’ll be under the guidance of a spine physical therapist who will guide you through a set of exercises. They’ll tailor the exercises to your condition and specific symptoms. A big part of success is maintaining the exercise routine they provide for you.
Some types of physical therapy used for treating chronic back pain might include:
- Testing your pain tolerance limits: Pain threshold and tolerance will vary from person to person.
- Retraining your posture: The physical therapist will show you the proper form and assist you in achieving the correct posture.
- Strengthening your core: Increasing core strength is important for decreasing back pain and reintegrating patterns of movement with better stability, awareness and bracing of your core.
- Conducting flexibility and stretching exercises: Flexibility and stretching exercises help reduce the tension in the muscles that support your spine, improve overall mobility and range of motion and reduce your risk of disability due to back pain.
- Doing aerobic exercises: Prolonged aerobic exercise can stimulate the nutrients and blood flow to your lower back, decreasing stiffness and encouraging healing.
5. Alternative Treatments
Some chronic back pain patients explore alternative treatments for chronic back pain. These include:
Acupuncture
Acupuncture can help treat chronic back pain. The specialist inserts thin needles into exact points throughout your body. Some specialists believe acupuncture can clear blockages in your body’s life force, which is referred to as Qi — pronounced “chee.”
Chiropractic Care
Different types of chiropractic care treatments many help with managing a chronic back pain like a herniated disc, for example. The treatment might involve manual adjustments where the doctor uses a sudden, controlled force to manipulate your joints to improve the quality and range of motion. Chiropractic care helps restore function and prevent injury as well as provides back pain relief.
Biofeedback
Biofeedback is a body-mind technique involving several types of monitoring devices for creating conscious control over our physical processes our bodies normally automatically control. Some processes biofeedback can affect in this manner could include breath control, heart rate, muscle tension, blood pressure and more.
Today, various types of biofeedback tools and instruments are available that show how effective this therapy can be and help monitor activity progress.
Yoga
Studies involving individuals with mild to moderate chronic back pain show certain yoga postures could decrease pain and improve your ability to move and walk.
Massage Therapy
The medical community is beginning to accept massage therapy as a credible treatment for various forms of back pain and as a supplemental therapy to use with other medical treatments. It offers several potential health benefits for individuals suffering from back pain, including:
- Reduced muscle tension: Massage therapy provides muscle relaxation helping to reduce pain caused by tight muscles, improve flexibility and even improve sleep.
- Improved circulation and blood flow: This brings nutrition to your tissues and muscles, helping in the recovery of muscle soreness from a soft tissue injury (like muscle strain) or physical activity.
- Increased endorphin levels: These are your brain’s “feel good” chemicals. Massage therapy enhances the mood helping to ease the anxiety and depression, often found in people with chronic back pain, which helps decrease pain and speed up recovery.
Behavioral Modification
Behavioral modification methods help optimize patient’s responses to painful stimuli and back pain. Cognitive therapy involves teaching a person to use coping techniques, relaxation techniques and other methods to alleviate back pain.
TENS
Transcutaneous electrical nerve stimulation (TENS) is a type of pain relief where electricity transmits through various parts of your body. Pain relief is a common reason individuals use TENS.
Through this therapy, your body receives mild electrical impulses. The TENS system is made up of a power machine, wires and electrode pads the doctor places on your skin close to the area that hurts. They then turn the unit on and send low-voltage electrical currents through your body.
TENs sessions typically last no more than 15 minutes and depending on the case, are performed as often as needed. Patients often report feeling a warm or mild tingling sensation during the treatments, temporarily preventing the individual from being aware of pain.
6. Surgery
Over 95 percent of our patients’ back problems are treated without surgery at Orthopedic Institute of Pennsylvania. However, when other treatments aren’t effective, doctors might turn to surgery to help relieve pain caused by severe nerve compression or musculoskeletal injuries. Surgery isn’t always successful, and there’s not a lot of evidence showing which surgeries work best for their certain indications. Individuals considering surgery need to know all related risks.
Surgical options may include:
Vertebroplasty and Kyphoplasty
These surgeries are minimally invasive and help repair vertebral compression fractures by osteoporosis. The doctor uses three-dimensional imaging during vertebroplasty to assist them in guiding a fine needle through the patient’s skin into their vertebral body — the biggest part of their vertebrae, the series of small bones that form your backbone.
With these surgeries, the doctor injects glue-like bone cement into your vertebral body space. The cement hardens quickly and helps strengthen and stabilize the bone, providing pain relief. In kyphoplasty, before you receive the bone cement injection, the surgeon inserts a special balloon and inflates it gently to reduce spinal deformity and restore height to your vertebral structure.
Spinal Laminectomy
The doctor performs this treatment when spinal stenosis is causing a spinal canal narrowing that causes numbness, pain or weakness. During the surgery, the surgeon removes the bony walls or lamina of your vertebrae as well as any bone spurs. The goal of this surgery is to open your spinal column up to remove pressure on your nerves.
Discectomy or Microdiscectomy
Your doctor might recommend discectomy to remove a disc, in situations where it has herniated and is pressing on the spinal cord or nerve root and causing enduring and intense pain. Microdiscectomy is a similar procedure, but it involves the surgeon making an extremely small incision in your back to remove the herniated disc, helping with more rapid recovery.
Foraminotomy
Foraminotomy is a surgery that enlarges or “cleans out” the foramen — bony hole — where your nerve root leaves the spinal canal. Joints thickened with age, or bulging discs can lead to narrowing of the space where your spinal nerve exits and may press on your nerve, causing numbness, pain and weakness. The surgeon removes small pieces of bone over your nerve through a small incision, so they can cut the blockage away and relieve the nerve pressure.
Intradiscal Electrothermal Therapy (IDET)

This is surgery for bulging or cracked discs due to degenerative disc disease. During the surgery, the surgeon inserts a catheter at the area of the disc in your back through a small incision. They pass a special wire through the catheter and apply an electrical current to heat the disc, helping to strengthen the disc wall’s collagen fibers, which reduces the bulging or other associated irritation of your spinal nerve.
Other surgical procedures may help with your chronic back pain in the event other treatments fail. You can sit down with an Orthopedic Institute of Pennsylvania provider for a consultation to discuss your treatment options.
Call the Orthopedic Institute of Pennsylvania to Make an Appointment for Your Chronic Back Pain

If you’re experiencing chronic pain or have been injured, it’s important you see a doctor to identify the source of your pain so you can have the best treatment for pain management.
At the Orthopedic Institute of Pennsylvania, providing caring and compassionate service is our priority. We strive to ensure we identify the exact cause of your pain so we can help you treat it properly. Chronic back pain shouldn’t be something you have to deal with every day. It’s our job to help alleviate your pain so that you can get back to living a better quality of life.
Visit here to view our providers in our eight convenient locations throughout Central Pennsylvania, or give us a call at 717-761-5530 to schedule an appointment.
Aches and Pains From Training, or Do You Have a Running Injury?
In this article:
- Are Body Aches and Pains From Training Normal?
- How Common Are Running Injuries?
- Signs You’re Overrunning
- Common Aches and Pains From Running
- Types of Running Injuries and Their Symptoms
- Treatment for Running Injuries at OIP
Wondering Why You Have Pain When You Run?
Running can be one of the most effective ways to directly benefit from exercise. Along with the potential to burn calories and lose weight, running can also benefit the body by improving cardiovascular and cognitive health. Many studies show consistent running can help an individual live a longer life. With a list of positive health benefits, it’s no wonder why running is a popular exercise that is part of a variety of training programs for a wide range of sports.
Those who integrate running into their daily or weekly exercise regimens may expose themselves to negative health impacts. Like all other forms of exercise, running can irritate or harm the body. Intense running, prolonged running or even improper running can cause the muscles and joints mild to severe damage. If you are feeling aches and pains throughout your body after training, and wondering, “Why do you have pain when you run?” it’s essential to determine the cause of the discomfort. Though some symptoms are common, others can be the result of a running injury.
The Orthopedic Institute of Pennsylvania is one of Central PA’s top health care practices. We take great pride in providing compassionate and caring service to patients suffering from pain associated with the injuries running and rigorous physical training can cause. Our physicians believe knowledge is key to responsible exercise, which is why we’ve identified common symptoms that may or may not be indicative of a running injury. If you experience lasting pain that may have been the result of a training injury, we encourage you to schedule an appointment.
Are Body Aches and Pains From Training Normal?

Although exercising does provide the body with many health benefits, part of this process does involve some pain or discomfort. Muscle soreness can be a positive sign that your muscles are beginning to grow and develop. However, soreness can also be a sign that your muscles or joints are negatively receiving stress that could lead to aches, pains and potentially even an injury. There are a variety of causes of running injuries:
- Poor form — If you are experiencing discomfort in your shoulders, back, arms or neck while running, your more significant could be the issue. Slight issues with your neck positioning, keeping your arms rigid or poor chest and shoulder posture could cause aches.
- Inadequate stretching — If you’re not properly stretching throughout any portion of your training program, you may begin to experience muscle soreness during or after your run.
- Incorrect footwear — Not only does your form influence your ability to run correctly, but your choice of footwear also impacts your performance. Shoes that are worn-out or old may no longer provide you with the support your muscles and joints need. Even new shoes can cause you discomfort if they do not fit correctly.
How Common Are Running Injuries?
Slight aches and pains are typical for those who integrate running into their training programs. Many of these symptoms are signs the body is improving in a healthy way. Unfortunately, even mild aches and pains could be symptoms of a much more serious health issue. Muscle and joint injuries are quite common among runners, and these ailments can range from temporary discomfort that requires rest to chronic pain that requires medical intervention.
Broadly, there are four separate categories of runners, based on the prevalence of their exercise. Marathon runners are the most intense of the group, and more than half these individuals suffer an injury each year. Only 32 percent of long-distance runners face running injuries annually, while 27 percent of novice runners incur injuries. However, novice runners are twice as likely to sustain an injury than those who run recreationally.
Regardless of whether an individual is focused on running or uses this exercise as part of their training regimen, all athletes can sustain an injury from running. Those who are beginning to run or are increasing their speed or distance may overextend themselves and cause physical pain. Even experienced runners and longtime athletes can suffer an injury due to overrunning.
Signs You’re Overrunning
Although exercise is healthy, too much exercise can be damaging to the body. Overtraining by overrunning could lead to minor aches and pains or major injuries to your muscles and joints. However, there are also other ways your body may alert you that your exercise routine is harmful. Signs that you may be overrunning include:
- Changes in mood — Too much exercise can cause the body to limit the production of certain hormones that help regulate your mood. Without these hormones, you may find yourself more irritable or stressed than normal.
- Frequent sicknesses — Improperly increasing the intensity or duration of your workout could negatively impact your immune system, opening your body up to the added potential of contracting viruses.
- Constant fatigue — Hormone changes that increase your stress level can also prevent you from getting the proper amount and quality of sleep you need, leaving you feeling regularly fatigued throughout the day.
- Trouble sleeping — Another way an excess of exercise impacts your body is by disrupting your body’s circadian rhythms, causing you to have trouble falling and staying asleep.
- Heaviness in the legs — Lack of sleep also prevents your muscles from healing correctly after each exercise routine. If you don’t give your muscles time to recuperate, you may feel soreness when you attempt to exercise again.
Common Aches and Pains From Running
There are many areas of the body where you may feel mild or moderate discomfort while running. Many of these symptoms will present themselves below the waist as pain in your legs, feet, thighs, shins, knees or ankles after running. Aches and pains may be apparent before, during or after exercise. Some discomfort may immediately dissipate when activity ceases, while other irritations may linger for days or weeks.
Runner’s Knee
Patellofemoral pain syndrome, more commonly called runner’s knee, is a common condition among those who engage in high amounts of cardio activity. Over-exercising or abnormal tracking of the kneecap could cause symptoms which include dull pains at the front of the knee and popping or cracking sounds when the knee is in motion. These symptoms can be apparent during exercise or regular daily activity.
Shin Splints
There is a close association between running and this common exercise problem, and runners especially are at a higher risk of feeling this discomfort. Shin splints can develop when novice runners overextend themselves as they begin exercising, or when consistent runners change the intensity or duration of their workouts. When the muscles, tendons and bone tissue around the tibia bone become stressed from overwork, they cause the runner to feel pain around the area where the muscles connect to the shin bone.
Sudden changes in the intensity of duration of physical activity can cause shin splints. Individuals who are naturally flat-footed or who are using inadequate footwear may develop this discomfort. Symptoms include sharp or dull throbbing during or after exercise and when touching the area. Shin splint symptoms may also be signs of chronic exertional compartment syndrome, which occurs when the pressure in the shin muscles builds.
Plantar Fasciitis
As the most common cause of pain on the bottom of the heel, plantar fasciitis results from the tissues on the arch of the foot becoming irritated and inflamed from damage or tearing. Though this can occur in any individual, certain risk factors like high-impact or increased activity can increase the likelihood of symptoms. Pain or discomfort usually occurs after exercise or after long periods of inactivity.
Muscle Strain
A muscle strain, or a pulled muscle, is a familiar muscular condition athletes and nonathletes can face. A strain occurs when muscles or tendons get stretched or torn. Most mild strains may include symptoms like pain, muscle spasms, swelling around the area or the inability to move the affected muscle. Muscle strains can occur in all parts of the body.
Though the issues above are common training injuries and causes of pain when running, their symptoms may also be signs of a more serious underlying problem. If you experience pain or discomfort in your lower extremities before, during or after your run, we suggest you consult a physician. The doctors at the Orthopedic Institute of Pennsylvania specialize in evaluating, diagnosing and treating joint, bone and muscular conditions runners and other athletes engaging in rigorous training may face. We invite you to contact us and schedule an appointment.
Types of Running Injuries and Their Symptoms
Runners can alleviate many of their aches and pains with minimal resources, and they heal in a relatively brief time. Some of these conditions won’t require the individual to alter their exercise routine heavily. However, larger issues like injuries may need more detailed treatment plans that could include surgical procedures.
Iliotibial Band Syndrome
IT band syndrome is a common cause of knee pain in those who exercise, and can be challenging to treat. Pain results when friction causes the band to become inflamed and begin to rub against the bone. Discomfort is typically between the hip and the top of the knee. However, because the pain can be challenging to pinpoint, a medical professional may mistakenly diagnose IT band syndrome as another injury like a lateral meniscal tear or stress fracture.
Achilles Tendonitis
Achilles tendonitis is a common condition in which the Achilles tendon becomes irritated and inflamed from repeated stress. Depending on which part of the tendon it affects, this condition could manifest in one of two ways. Noninsertional Achilles tendonitis causes the middle portion of the tendon to tear, swell and thicken. Insertional Achilles tendonitis affects the lower part of the tendon and may cause bone spurs. Both forms of Achilles tendonitis may also cause the tendon fibers to calcify.
Stress Fractures
Stress fractures are some of the most common injuries athletes face due to overuse. Increased frequency or intensity while running or doing other forms of cardio can cause these fractures, as can other stressors like hard surfaces, improper equipment and added stress on the bones. More than half of stress fractures occur in the bones of the lower leg, placing runners at an increased risk. Pain is present during activity and recedes with rest. Untreated stress fractures could become breaks if runners place more stress on the area.
How to Tell the Difference Between a Running Injury and Normal Discomfort From Running and Rigorous Training
It can be difficult to determine whether the discomfort you’re feeling during or after your workout is a typical case of muscle soreness, or if you’ve sustained an injury. Though each case is unique, some features can help you begin to distinguish injury pain from soreness and discomfort.
Features of Aches and Discomfort
- The sensation is tender and burning during exercise, but dull at rest.
- The onset of the pain occurs during exercise or within the first one to three days of exercise.
- The feeling lasts for two to three days before getting better.
- The pain is only in the muscles.
Features of Pain
- The sensation is sharp and acute at rest and during exercise.
- The onset of the pain occurs during exercise or within the first day of exercise.
- The feeling does not lessen or go away on its own.
- The pain is in the muscles, as well as deeper in the joints.
Each person has a different tolerance for pain, and because many of these injuries could be masking themselves as mild soreness, it’s crucial to assess your symptoms before exercising again. If you believe your aches could potentially be a running injury, ask yourself the following questions:
- Has your performance suffered because of the pain? Everyone has an off day, and it’s natural that your body may perform amazingly one day and averagely the next. However, if you see your performance consistently suffering as a result of this pain, it may be an injury. For instance, if your typical routine involves a five-mile run, but pain in your knee or lower leg prevents you from achieving that milestone, you should consult a physician.
- Do you alter your stride to compensate for the pain? If you’ve had to change your gait to lessen the pain or its impact on you, you may have an injury. Not only is the untreated injury impacting your form, continuing to run improperly could cause new injuries to occur.
- Does the pain remain consistent or increase while running? It’s natural to feel a little tight or sore as you start your run, especially if you frequently train rigorously. If these aches don’t subside or become painful as you continue running, this may be a sign that there’s an underlying injury. Consider contacting a doctor if you have tightness or leg pain after running.
- Are your legs sore or swollen? Soreness and swelling are common after intense workouts, but when sharp pain accompanies swelling, it could be a symptom of much more. Always be aware of any inflammation that does not recede quickly.
- Does the pain stick with you when you’re walking normally? Although it’s natural to feel a little sore right after your workout, your body should recover quickly enough to allow you to return to your daily activities. If you’re having trouble walking around naturally or cannot complete daily activities because of the pain you feel, you could have a severe injury.
Treatment for Running Injuries at OIP

Those who integrate running into their exercise routine should expect to feel some level of discomfort during their training. Though many aches and pains of the muscles, bones and joints can be common, some of these symptoms can also be warning signs that a more serious injury has occurred. It’s essential for individuals who participate in all activity levels to know how to recognize the difference between ordinary discomfort and unusual pain. Thankfully, the specialists at Orthopedic Institute of Pennsylvania have the knowledge and experience to diagnose and treat these conditions.
Our team of compassionate doctors is prepared to treat your injuries through a variety of surgical and nonsurgical treatment options. We’re proud to provide care for fractures, pain management and orthopedic injuries to the knees, feet, ankles, spine and more. Visit our website to learn more about our services and the talented physicians who have cared for families throughout Central Pennsylvania for years. We service patients throughout the region with our practices conveniently located in Camp Hill, Harrisburg, Carlisle, Hershey, Millersburg and Newport.
Don’t risk causing further harm to your body by neglecting a running injury. Call Orthopedic Institute of Pennsylvania today to schedule an appointment with a physician and identify the cause of your pain.
Ice vs. Heat for Injuries: How Do I Know Which Is Best?

In this article:
What’s better for inflammation, heat, or ice?
Everyone experiences pain. Whether it’s a headache, a torn ligament, a sprained ankle or sore muscles, pain is just a fact of life for many people. Pain is our body’s way of telling us when something is wrong, whether it’s a new injury, a medical condition or the result of a long day on our feet. However, pain is not something anyone needs to tolerate.
Whatever the reason for pain, one undeniable fact remains: No one wants to be in pain. And, while modern medicine has produced a lot of reliable medications that are designed to help with various levels of pain, it’s not always necessary, or appropriate, to rely solely on medication to correct the problem.
That’s where ice and heat therapies come in. Depending on the source of your pain — arthritis, a new injury or a grueling workout — ice, heat or both can go a long way toward relieving your pain and improving the overall quality of your life.
Yes, we know most people are aware of this. And, if you’re like most people, you’ve likely got an ice pack stashed in your freezer and a heating pad tossed somewhere under your bathroom sink. But, do you know when to ice muscles vs heat them? Unfortunately, there is a lot of confusion out there over how to use them. Not only that, but if you choose wrong, you can make your problem worse, instead of better. Knowing how to use these two options for pain relief can go a long way in easing your pain and improving your comfort, whether you’re dealing with an injury or an ongoing chronic condition.
Heat for Injuries

While there’s no substitute for consulting with a doctor when pain occurs, having the knowledge to treat yourself can help you to stay more comfortable while you’re waiting for an appointment. Heat therapy is an excellent option because you can do it safely, effectively and easily at home.
The goal of heat therapy is to improve circulation and blood flow to raise the temperature around a specific area that has been injured or is experiencing pain of some kind. By increasing the temperature and improving circulation, heat can relax injured muscles, heal damaged tissues and improve flexibility.
Not only can heat calm pain flare-ups, but it is an excellent way to soothe muscle tension, stiffness and even chronic back pain. Muscle tension can spiral into many other problems, including headaches, which also cause pain. Relying on heat to relax your muscles can also relieve a lot of pain caused by stress and anxiety, in addition to chronic conditions or injuries. There’s a reason so many people swear by a relaxing hot bath or a stint in a sauna to improve their overall health and well-being.
How to Use Heat
You can administer heat therapy in two different forms: dry heat or moist heat. Dry heat is the kind that comes from heating pads or saunas, while moist heat comes from sources like steam towels or a hot bath or shower. Typically, when you’re using either form of heat therapy, you’ll only apply it to the specific part of your body that is in pain. The exception to this, obviously, is a hot shower or sauna, which tend to target your whole body. Of the two options, moist heat works faster, which means you won’t have to apply it as long as you would a dry heat. However, it can be messier, so it may not always be the best option.
As an aside, there are many different kinds of heating pads out there. If you opt to use an electric one, just make sure you don’t fall asleep while it’s on, or select one that has an automatic shutoff feature instead of remaining on until you switch it off.
When to Use Heat
Because the goal of heat therapy is to soothe and heal damaged tissues, it’s best to use heat when you are dealing with muscle pain or soreness. Doctors often recommend it to treat chronic muscle pain rather than a new injury — we’ll explain more about why later on. That’s not to say putting heat on an injury is out of the question — however, never apply heat to a new injury that is still swelling. Heat will make the swelling and pain worse, which is not what you want. You also should not apply heat if your body is already hot — for example, if you’re sweating. It won’t be effective.
One of the benefits of heat therapy is that you can apply it for longer than you can use ice. For minor aches and muscle tension, apply heat for 15 to 20 minutes at a time. If you’re treating more severe or widespread pain, longer heat sessions — such as a bath or sauna — may last from 30 minutes up to two hours.
We’ve said it before and we’ll say it again: Heat is an excellent way to ease pain and relax muscles. However, if you find yourself relying on heat over a long period without decreases in your pain levels, consult with your doctor. Heat is a good tool, but it’s not a substitute for necessary medical intervention.
One question many people have is whether it’s safe for pregnant women to use heat therapy. Because doctors advise against the use of hot tubs and saunas while pregnant, some people are worried even using a heating pad could be dangerous for women who are expecting a baby. That is because there are concerns over raising a pregnant woman’s body temperature and how it can affect the baby.
However, localized heat therapy is an excellent way for women to cope with the muscle aches and pains they experience during pregnancy, especially low back pain and muscle spasms. It doesn’t significantly raise a person’s core temperature, and there is absolutely nothing wrong with using a heating pad or moist towel to ease the inevitable pain that accompanies your increasing abdomen. Pregnant women should never apply heat directly to their abdomens, and, as we mentioned previously, pregnant women should always avoid full-body heat therapy like saunas or hot tubs.
Ice for Injuries
Unlike heat therapy, the goal of cold therapy is to slow circulation and blood flow to an infected area. It can reduce swelling and inflammation from an acute injury — that is, an injury that just happened — which in turn decreases pain and discomfort. That is because the cold also temporarily reduces the nerve activity around the affected area. Ice can also be an excellent option for someone who works out a lot, because an intense workout can cause swelling and pain.
How to Use Ice
Most of the time, ice therapy comes in one of four forms:
- Ice massage
- Ice packs
- Ice baths
- Coolant spray
In more extreme cases, your doctor may recommend using a cold therapy chamber, cryostretching or cryokinetics. But, you’ll typically need to do those activities under the observation of a medical professional, not on your own. For our discussion, we’re going to focus on the most common forms of ice therapy you can do in the comfort of your home.
Apply a cold pack directly to an affected area for a localized impact. Sometimes, you may need to use ice on a wider area or even your whole body — this is where an ice bath or massage may come in.
If you have wondered why ice hurts on your injury, you are probably making this common mistake. When you’re applying ice locally, make sure to wrap your ice pack in a towel. It should never directly touch your skin because the cold will hurt you. Unlike heat, you should only apply ice for short periods, though you can space out your sessions several times a day. In general, doctors recommend using ice therapy for 10 to 15 minutes at a time. Elevating the area you injured can also improve results. You can use a medical ice pack or, if one isn’t on hand, you can improvise with a bag of frozen vegetables or a plastic bag full of ice.
When to Use Ice
If you’re wondering, “Should I ice my injury?” here’s some additional advice. It’s best to use ice when an injury first happens, especially if you experience bruising and swelling at the site of your injury. Because it slows blood flow and circulation, ice can reduce bruising and swelling, which helps with pain and healing. Medical professionals don’t typically recommend ice for chronic muscle pain, although, as we’ll talk about later, there are exceptions to this rule.
Unlike heat, however, ice is not for everyone. It can cause some serious problems if people use it too much or incorrectly. People who have a sensory disorder that might prevent them from sensing pain shouldn’t use ice therapy without a doctor’s supervision. That’s because they may not be able to feel it if they leave the ice on their skin for too long, and then it may damage their skin. People who have cardiovascular disease, heart disease or issues with poor circulation should also avoid using ice therapy if they haven’t consulted with their doctor first.
Ice can also make your pain worse if you misuse it. For example, if your body is already cold, it will interfere with your ability to get warm, and it will also not effectively control and reduce your pain. Ice can also make your pain worse if you mistakenly use it to treat a tight muscle because it will make the muscle tighten and contract more, rather than relaxing it and easing the tightness that’s causing the pain. Sometimes this happens when people incorrectly identify the source of their pain. For example, this is common in people who struggle with pain in their neck or low back. They mistakenly apply ice to the affected areas, causing their muscles to tighten and spasm more instead of relaxing their muscles, which is what heat would do.
Should I Use Ice or Heat? How to Choose
Ice or heat: Which is better for an injury? We could fill pages with all the different scenarios where you might have to decide whether to use heat or ice to treat pain. But, as a general rule of thumb, we recommend this: If it’s bleeding or swelling, start with ice.
Depending on the extent of the injury, you may also want to go ahead and call your doctor. But, if you opt to wait, use ice for 48 hours. Then, if it’s still swollen and painful, definitely make a doctor’s appointment. This rule holds true even if you suspect you have injured a muscle.
What’s better for inflammation, heat, or ice?
Some other common questions are if heat can help heal a pulled muscle, or how long you should apply heat to the injury. While heat may be beneficial in the long term to heal the pulled muscle itself, ice may initially be the best treatment for the injury to reduce inflammation and the pain it causes.
If you’re sore or achy, start by applying localized heat to the area that’s bothering you.
Pay close attention to how your body reacts to the application of heat. Does your pain go away with a heating pad? If it doesn’t go away or the pain gets worse, stop using heat and call your doctor to set up an appointment to discuss the cause of your pain. Even if the heating pad does ease your pain, keep a close eye on how often you use heat to control your pain. If it becomes something you rely on a lot, you may still want to talk with a doctor about what’s causing your ongoing pain.
Sometimes doctors recommend alternating between ice and heat therapy, which is called “contrasting therapy.” One instance where this is a common recommendation is in patients with arthritis. Heat therapy can ease the joint stiffness that accompanies arthritis, while ice can treat swelling or acute pain that presents itself. Over time, someone who is suffering from arthritis may learn how to use both therapies to ease their pain, but only after consulting with a doctor.
We’ve said it before, but it’s worth repeating: Never use ice or heat therapy as an alternative to consulting with a doctor. Whenever you experience a significant injury or ongoing pain, it’s crucial to consult with a doctor you trust.
When Ice or Heat Isn’t Enough
If you have been injured or are experiencing chronic pain, it is essential to see a doctor, not only to discuss pain management, but to properly identify and treat the source of your pain.
Sometimes people try to avoid going to the doctor when they are in pain because they have had a bad experience. They may have been misdiagnosed or misunderstood. They may have seen a doctor who didn’t take the time to answer your questions. Or sometimes people are just afraid of what a doctor will find. At the Orthopedic Institute of Pennsylvania, our priority is compassionate and caring service. Our job is not to be right — our job is to identify the source of your pain and assist you on the journey to addressing and treating your pain. Pain should never become a lifestyle.
Based in Central Pennsylvania, we are proud to be a part of several medical partnerships that provide care and treatment to the residents in and around our service area. If you are experiencing pain, whether it began recently or has been ongoing for some time, contact us today and find out how the Orthopedic Institute of Pennsylvania can help you recapture a pain-free life.
College Football Day
We celebrated our favorite college football teams recently! Check out the pictures to see if your favorite team was represented!











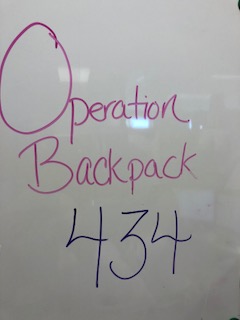
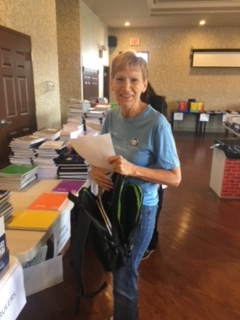
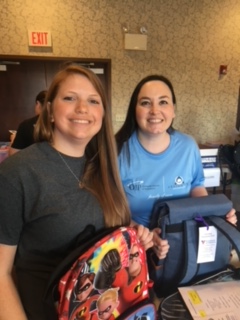
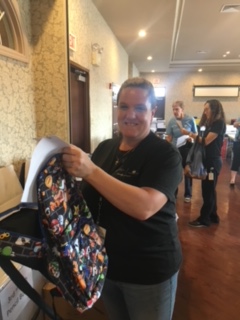
Operation Backpack Total
We would like to thank all who contributed to Operation Backpack in any way! In total we were able to donate 434 backpacks along with countless amounts of school supplies! Our goal this year was 300 and we clearly surpassed that! Thank you again, we are looking forward to crushing this number next year as well!



IMG_7218



