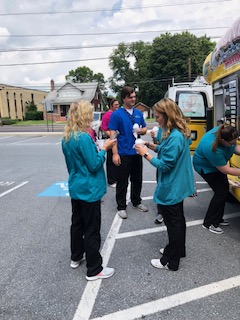
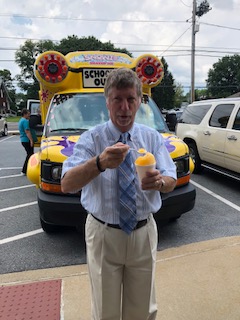
Mr. Sno- Cone
Mr. Sno-Cone stopped by all of our locations to celebrate our employees! Check out the pictures below!
























ABC27 Operation Backpack
We were featured on ABC27, 5:30 show on 8/1.
We were given the chance to speak on behalf of our fundraiser for Operation Backpack!
You can check out the video here:
https://www.abc27.com/news/local/harrisburg/operation-backpack-readies-students-for-school/1340079867
Orthopedic Institute of Pennsylvania Announces New Doctor
Orthopedic Institute of Pennsylvania
3399 Trindle Road
Camp Hill, PA 17011
717-761-5530
FOR IMMEDIATE RELEASE
July 9, 2018
Orthopedic Institute of Pennsylvania Announces New Doctor
Anesthesia and Perioperative Medicine and Pain Management doctor is the newest addition to team of providers
CAMP HILL, PA. – The Orthopedic Institute of Pennsylvania, a leader in family care, is pleased to welcome Taryn Reichard, DO, to the active medical staff.
Dr. Reichard is originally from the Harrisburg Area, graduating from Central Dauphin High School. She then went on to attend Robert Morris University in Pittsburgh, PA where she played Division -1 soccer and completed her bachelor’s degree. She completed medical school at the Philadelphia College of Osteopathic Medicine in Philadelphia, PA. Following graduation, she completed her residency in Anesthesiology and fellowship in chronic pain medicine at Penn State Milton S. Hershey Medical Center.
Dr. Reichard is board certified in Anesthesia and Perioperative Medicine and Pain Management. She holds memberships with the spine intervention society, the American Academy of Pain Medicine, and the Pennsylvania Pain Society. She is a program committee member for the American Academy of Pain Medicine.
Dr. Reichard resides in the Harrisburg area with her husband and rescue dog, Faith. She enjoys all the benefits of being close to family and friends, and loves traveling, hiking, running, and trying new restaurants.
Dr. Reichard will be seeing patients in our Carlisle and Hershey offices. To schedule an appointment with Dr. Reichard, call The Orthopedic Institute of Pennsylvania at 717-761-5530. Appointments are available beginning July 31st.
###
Operation Backpack
Once again we will be participating in Operation Backpack!!
We will be accepting donations now through August 3rd. Last year the doctors and employees donated 201 backpacks, supplies and cash donations!
Patients can drop off supplies and backpacks at any of our locations in the lobby!
Again, the doctors will be matching backpack donations! Below is a list of most needed items!
Let’s get donating!!
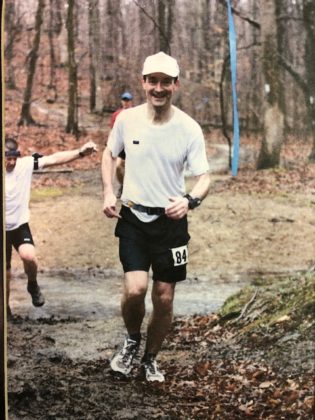
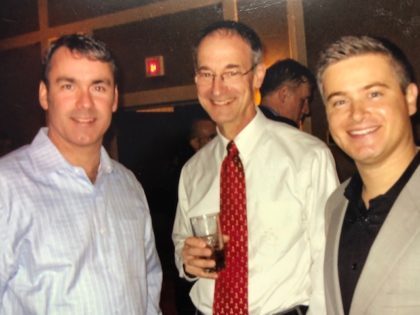
Dr. DeMuth – Retirement
On behalf of The Orthopedic Institute of Pennsylvania we would like to Congratulate Dr. William W. DeMuth on his retirement!
His patients compliment him on his personable bedside manner and the compassion he shows. With these attributes and his medical expertise and orthopedic skills, he has successfully created positive, memorable experiences for his patients and their families – part of OIP’s mission.
We recently celebrated his retirement and it was an evening to recognize all of Dr. DeMuth’s accomplishments during his time here at OIP!
Thank you for your commitment to OIP, Dr. DeMuth. You will be missed!





Preventing and Treating Heat Exhaustion
Removing excess heat is a normal function of the human body. This is accomplished by pumping blood close to the skin’s surface, which causes the release of sweat. This usually works, until warmer, humid weather makes it a little harder to do so. When the air becomes warm and moist, the air will absorb a lot less sweat from the skin. It will also hinder the human body’s capability to cool itself down by sweating.
When we become dehydrated, it means our bodies are lacking water and electrolytes, which are vital salts. Dehydration lessens our sweating capabilities. If we are not able to cool ourselves through sweating, we might experience heat exhaustion. Heat exhaustion will raise the body’s temperature.
In the hot seasons, millions of people are exposed to the dangerously high temperatures every year. Laborers who work outside make up the biggest segment of patients who seek medical treatment for heat-related illness. The next largest segments of those who are often affected by heat-related illnesses include the elderly, young children and athletes. Heat-related illnesses are almost entirely preventable. Doctors can do a lot to educate their patients on how to remain safe during the hot months.
What is Heat Stress?

Sometimes, human bodies become so hot that they cannot regulate body heat adequately. According to OSHA (Occupational Safety and Health Administration), if this occurs, the body’s internal temperature starts to go up over the standard 98.6 degrees Fahrenheit. The rising temperature strains the body. This is heat stress. Heat stress symptoms are classified into levels of heat-related illnesses, or HRIs. Each category depends on the HRI’s severity.
Treat heat stress early to avoid it escalating to heat exhaustion. Heat stress, if ignored, will escalate quickly to heat exhaustion, and then into the more severe territory of heat stroke.
It is crucial to your well-being to be aware of how you feel if you’re outside in the sun. Be sure to consider your symptoms. If applicable, evaluate the symptoms of the people around you. Prompt medical attention can ward off heat exhaustion and its damage. Untreated heat stroke can cause damage to organs, your brain and other tissues.
Symptoms of Heat Exhaustion
Heat exhaustion symptoms vary. They could include sweating excessively, headaches and dizziness. Overlooking these symptoms is a little too easy sometimes, as they can mimic those of several other medical conditions.
Common signs of heat exhaustion to look for:
- Excessive sweating
- Headache
- Dizziness
- Nausea
- Vomiting
- Increased internal body temperature
- Rapid or weak pulse
- Low blood pressure
- Lightheadedness upon standing up or bending over
- Muscle cramps or weakness
- Pale, cold skin, possibly damp
- Goosebumps
- Aggressive or irritable behavior
- Reddish, flushed face
- Shallow, rapid breathing
Causes of Heat Exhaustion and Other Contributing Factors
Warm, humid weather combined with demanding, outdoor labor often are the culprits of heat exhaustion. Other factors can increase the likelihood of heat exhaustion.
- 60 percent or higher atmospheric humidity level
- Conditions of the kidney or liver
- Intense physical labor
- Diabetes, hyperglycemia or other conditions that increase the chances of being dehydrated
- Drug abuse
- Alcohol use, long-term or heavy
- Smoking
- Being obese over overweight
- Medications for depression, insomnia or poor circulation
- Hypertension or high blood pressure
- Cardiovascular or heart disease
- Being younger than 4 years old or older than 65 years old
The factors that will put a child at risk for dehydration are the same things that will put an adult at risk for dehydration: extended exposure to the direct summer sun, elevated humidity levels and high temperatures without drinking enough fluids or getting enough rest.
Complications Caused by Heat Exhaustion
On its own, heat exhaustion is not painted as a serious health concern. However, if it is left untreated, heat exhaustion may escalate to heat stroke, which has severe complications. These include organ failure and brain damage. Heat exhaustion can cause a serious health risk when intense physical activity is continued without addressing symptoms. Complications of heat exhaustion may include:
- Serious injury to kidneys
- Rhabdomyolysis, the breakdown of muscle fibers which may lead to kidney failure, dark urine, vomiting and muscle aches
- Liver failure
- Arrhythmias, an uneven or overly fast or slow heartbeat
- Coma or delirium
How To Prevent Heat Exhaustion — Can It Be Avoided?
There are several ways to avoid heat illnesses. Here are some very useful tips for how to combat heat exhaustion. Keep them in mind.
The best way to avoid heat exhaustion is to stay cool and hydrated. If possible, stay inside in air-conditioned areas when the temperature is high. If you have to go outside, take precautions, such as the following:
- Wear light-colored, lightweight, loose-fitting clothing. Light colors reflect heat and sunlight and absorb less heat than dark colors.
- Wear a large-brimmed hat or use an umbrella to protect yourself from the sun.
- Apply sunscreen with an SPF of 15 or higher.
- Drink water often during daylight hours to avoid dehydration.
- Sports drinks like Powerade and Gatorade can assist in restoring electrolytes if necessary.
- Avoid caffeinated drinks such as coffee, tea and soda, as well as alcohol.
- Outdoor activities should be rescheduled for cooler times of the day. Usually, this is before 10 AM and after 6 PM.
- Take several breaks from outdoor activities taking place in heat and humidity.
- Never leave a child, a pet or yourself in a car when it is hot. Even if windows are open, the heat can become severe and dangerous rapidly.
How Do We Treat Heat Exhaustion?
There are some things you need to do if you suspect someone has a heat-related illness. The following tips on how to cure heat exhaustion symptoms should be very useful in trying to prevent heat exhaustion from escalating into heat stroke.
- Quickly get out of the heat and into a cool place. If air conditioning is not available, at least get into the shade.
- Lay down, elevate your legs and feet so that blood will start flowing to your heart.
- Remove any tight or extra clothing.
- Soak some towels in cold water and apply them to your skin.
- Take a cool bath or, if you are strong enough to stand up, a cool shower.
- Sip, do not chug, water or sports drinks. Do not drink caffeinated or alcoholic beverages.
Remember to Protect the Vulnerable From Heat Illness
The most vulnerable to heat illnesses are the elderly, children, and babies. They are a lot more sensitive to heat and should be afforded more attention than usual in the hot months. Older people do not adjust to abrupt changes in temperature as well as they did when they were younger. They have a higher chance of having a chronic condition that affects how their bodies respond to heat or of being on medication that decreases their ability to control their core temperature or their ability to sweat.
If you have elderly neighbors, friends or relatives, you can help protect them from heat-related illnesses by doing the following:
- Keep them in mind. Visit elderly adults who are at risk at least twice a day. Check for signs of heat exhaustion or heat illness.
- Be sure to encourage your elderly friends and relatives to drink more fluids such as water and other cool, alcohol-free beverages. Do this even if they aren’t particularly active or athletic.
- Important note: If their medical professional has limited the amount of liquid they drink, or if they are on diuretics, they will need to consult with their doctor to see how much they should drink if the weather becomes hot.
- If they do not have air conditioning where they live, bring them to an air-conditioned location such as a cooling center if they have issues with transportation.
Protect Children From Heat Exhaustion
The long summer days are filled with activities for kids. From camps to organized sports, kids are outside a lot. Even spending days at the local pool can increase a child’s risk for heat illness. Children are at higher risk for heat exhaustion than adults because their bodies have less surface area compared to their weight. This makes it more difficult for heat to leave their skin. The best thing you can do to prevent heat exhaustion in children is to proactively make sure they do not become dehydrated.
First and foremost, make sure they drink early and often. Cold water is the best option. When your child goes to play, send them to their activities fully hydrated. While they are playing, see that they take periodic breaks to drink something, even if they claim they aren’t thirsty. An appropriate size drink for a child is about five ounces if a child weighs 88 pounds.
Signs of dehydration in children are similar to those of adults. Look for tiredness, low energy and dry lips. If a child says he or she is thirsty, they are most likely already dehydrated. Get them to sip water or a sports drink immediately. If your child becomes heat exhausted, immediately stop their play, bring them into a cool or shady area, and treat them with the same tips listed earlier used for adults.
What is Heat Stroke?
Heat stroke is the most severe heat illness. Heat-related illness is classified as heat stroke when the core body temperature is over 104 degrees Fahrenheit. If you think someone has heat stroke, immediately call 911 or get them to a hospital. In the meantime, treat their symptoms the best you can.
Heat stroke can damage brain cells and other internal organs. It mostly affects people over the age of 50, but has also sickened young athletes who are otherwise fit and healthy.
Escalation from heat exhaustion is usually how heat stroke or sunstroke develops. It often starts with a mild heat-related illness like heat stress and escalates to heat exhaustion. What is most worrisome is that heat stroke can often present itself suddenly with no previous signs of heat illness at all.
A combination of dehydration and extended exposure to high temperatures leads to heat stroke. It can lead to the body’s temperature regulation system failing. Above 104 degrees Fahrenheit, the nervous system develops complications after being exposed to this very high temperature.
Symptoms of Heat Stroke
Fainting is usually the first sign of heat stroke.
Other heat stroke symptoms include:
- A headache that throbs
- Light-headedness and dizziness
- Not sweating even in hot weather
- Dry, hot, reddish skin
- Cramps or muscle weakness
- Nausea
- Vomiting
- Rapid heartbeat
- Shallow, rapid breathing
- Confusion or disorientation
- Seizures
- Unconsciousness
Risk Factors for Heat Stroke
Older adults whose homes lack air conditioning or proper ventilation are most likely to be affected by heat stroke. Other people who are at high risk of heat stroke include those in any age group who do not drink enough fluids, who have chronic ailments or who drink too much alcohol.
The heat index is strongly linked to heat stroke risk. The heat index measures how hot it feels when relative humidity and temperature are calculated together. Remember, a humidity level of sixty percent or higher hinders the evaporation of sweat, which diminishes your body’s ability to cool off.
When the heat index reaches 90 degrees Fahrenheit, the risk of heat illness increases substantially. This is why it is so important to take note of the daily heat index and to note that being in full summer sun increases the reported index by up to fifteen degrees.
Other risk factors for heat stroke include:
1. Age
Again, children under 4 and adults over 65 are slower to adjust to heat than other people.
2. Health issues
Many health conditions increase your risk of heat stroke, including:
- Being obese or underweight
- Having diabetes
- Having hypertension or other heart diseases
- Having respiratory or kidney disease
- Having a mental illness or mood disorder
- Abusing alcohol
- Having a condition that causes fever
3. Medication:
These medications can increase the risk of developing heat stroke:
- Antihistamines
- Diet Pills
- Diuretics, sometimes called water pills
- Sedatives
- Stimulants
- Seizure medications or anticonvulsants
- Heart and blood pressure medications
- Antidepressants or antipsychotics
- Illegal drugs like cocaine and methamphetamine
Preventing Heat Stroke
The steps to prevent heat stroke are similar to the prevention steps for heat exhaustion. Mainly, stay hydrated, wear loose, light-colored clothing, try to avoid arduous physical activity in direct sunlight, and take note of the heat index for the day.
When Should You See a Doctor?
Left untreated, heat exhaustion can lead to heat stroke. Heat exhaustion does not affect and impair mental function, cause loss of consciousness, or confusion. Heat exhaustion will not cause a person’s body temperature to go over 103 degrees Fahrenheit. If a person faints or loses consciousness, has a temperature over 104 degrees Fahrenheit, is experiencing extreme nausea, vomiting, seizures, or any of the listed heat stroke symptoms, immediately seek medical assistance for that person.
Get the Information You Need
For more information on how to safely navigate your summer, check out our other articles. The Orthopedic Institute of Pennsylvania is dedicated to providing exceptional care to our patients. We offer a holistic approach to all your orthopedic issues, and many of our providers are specialists in case you need more specialized care. We have a variety of services and treatments and are proud to say 95 percent of our patients never need orthopedic surgery to cure their problems. Request an appointment today at one of our eight convenient locations.
PSFCA BIG33 Football Classic
Over the weekend we were a sponsor of the PSFCA BIG33 Football Classic! We had a push-up competition at our booth, met a lot of great people, and watched a fun game of football! Thank you to all who came out and supported!





Injury Prevention for High School Athletes
Some 30 million kids play some type of organized sports in the United States. More than 10 percent of them, some 3.5 million, will experience an injury at one point or another.
There are many benefits for teens who participate in sports. These benefits are immediate and extend far into the future. Playing sports on a team or individually not only provides excellent exercise opportunities but also helps to prevent obesity and chronic health problems. Sports also teaches the concepts of teamwork, discipline, strategic thinking, and improved self-confidence.
Luckily, there are ways these injuries can be prevented. Read on to learn why injuries can impact an athlete beyond the physical consequences and what steps parents in Central PA can take to keep their teen athletes’ injuries to a minimum.
Negative Effects of Injuries

When a young athlete becomes injured, it can cause significant levels of stress and setbacks for the teenager and their support system. It may affect their family, coaches and teammates. The pressure felt by the high school athlete to perform could even prolong the impact of the injury in unexpected ways, such as:
- Time “Lost” Due to Injury: The athlete not only has to deal with the injury but could lose time at school, at practice and with their friends. It’s possible they might miss a whole season.
- Shattered Expectations: Family, coaches, and the school’s community can project a lot of their expectations upon a team’s young players. An injury will immediately put a negative tinge on these hopes and aspirations.
- Lost Scholarship Opportunities: Student-athletes seeking out athletic scholarships may have their future plans fall apart when they are injured. With everything up in the air, added stress becomes part of the healing process, which isn’t good for a teenager, especially one who is trying to heal.
Athletes can obtain additional injuries that take years to fully heal because they continue to play without letting the original injury heal properly. These injuries may lead to problems during adulthood, requiring one or more future surgeries. In many cases, arthritis becomes a problem later down the road when there isn’t proper medical treatment or healing for an extended period of time.
It is essential to seek proper medical attention immediately when a sports injury occurs. To make certain the best possible healing and recovery happens, athletes, their parents and their coaches need to follow best practices, so they can get back to playing again sooner rather than later. Your athlete should strive for high school athletic injury prevention.
The Most Common Classifications of Injuries Among High School Athletes
The most common injuries for high school athletes vary. Different types of injuries depend on several factors, including the parts of the body affected and the different sports they play. Awareness of possible injuries can help us learn how to better prevent or lessen injuries in high school athletes. The most frequent types include:
- Acute injuries
- Overuse injuries
- Catastrophic sports injuries
- Concussions
- Growth plate injuries
Let’s take a look at seven of the most prevalent injuries to high school athletes and how to prevent them.
Injury 1: ACL Damage
One type of knee injury is when damage occurs to the ACL, or the anterior cruciate ligament. Considered a severe injury, this happens mostly to football players and those who participate in other contact sports. Doctors are seeing more and more adolescents and teens with ACL injuries than they saw just two decades ago.
They note young people start sports much earlier in life while pushing themselves harder than they used to so they can stay competitive. Another cause for the rise in ACL injuries in younger athletes is they focus on just one sport, which puts their knees at high risk for injury with repeated motions.
ACL injuries concern medical experts because surgery is not an easy fix for teens. It is more difficult to repair ACLs in teens than in adults. ACL reconstructive surgery in younger people can cause unevenness in the lengths of their legs or other complications. Yet opting to skip surgical repair can result in other problems such as early arthritis symptoms.
How to Prevent ACL Damage
Strengthening the knee, hips and thighs offers one way to guard against an ACL tear. Have your teen do squats, lunges and core moves to improve strength in these areas.
Proper warm-ups before athletic activity can limber up the ACL before activity. Emphasize to your teen the importance of jogging and stretching prior to games and practices.
Finally, encourage kids to keep an awareness of their knees while playing. Watch for the knee collapsing in. Have them practice keeping the knee lined up above the foot when they jump, run or stop suddenly.
Injury 2: Runner’s Knee
Runner’s knee is a blanket term used for describing conditions that affect the knee. It occurs most among runners because of overuse. They happen in athletes who do a lot of activity that requires bending of the knee, like bicycling, skiing or jumping. Runner’s knee stems from a misaligned kneecap. When it rests off track, it causes pain because it does not slide smoothly.
Signs of runner’s knee include pain and tenderness behind the kneecap or on either side of the kneecap toward the backside and middle of the knee. Also, there may be swelling of the knee. Pain will generally present when bending the knee while walking, kneeling or running. Sitting with your knees bent for a long time can spark pain as well. If left untreated, this condition can damage knee cartilage and lead to arthritis in the knee.
How to Prevent Runner’s Knee
Teens can employ a number of different tactics to guard against runner’s knee, including:
- Strengthening the knee with exercises similar to those used to prevent an ACL tear
- Changing their running gait, which could reduce stress on the knee
- Not building up running mileage too quickly
- Taking a break from exercise when knee pain flairs
Injury 3: Concussions
These are injuries to the brain of a traumatic or mild nature, depending on the severity. Concussions happen when someone takes a hit to the head or body. The blow causes forceful movement of the brain in the skull.
Signs and symptoms of concussions are divided into four different categories:
- Physical
- Cognitive
- Emotional
- Sleep-related
A headache is the most widely reported symptom of a concussion. Another symptom of a concussion is amnesia. Symptoms of concussion can also mirror depression, anxiety and attention-deficit disorders. If a teen already has any of these disorders, a concussion can make the symptoms worse and harder to control. Teens with learning impairment issues and other cognitive delays may also show the same symptoms. This also makes treatment and management of a concussion more difficult.
Concussions can occur in all sports, but they happen most frequently in girls’ soccer, basketball and volleyball, as well as boys’ football.
How to Prevent Concussions
Here are a few tips on how to prevent concussive injuries in high school athletes:
- Choose the Right Protective Gear: Make sure your teen wears the appropriate headgear for their sport. The headgear should fit properly. Don’t forget about safety equipment when participating in non-contact sports, such as biking, skateboarding, rollerblading, snowboarding or skiing. Helmets and other headgear prevent damage from concussions. Helmets and mouth guards can reduce the risk of injury to the brain.
- Stay Aware: Helmets and head protection are the first line of defense against concussions. That said, concussions can still occur because protective headgear doesn’t stop injuries. If you hit your head, your brain can still move about and get injured by skull impact, even with a helmet on. Teach your teen to make smart choices on the field that put them in less danger of sustaining a hard blow.
- Don’t Take Chances: Tell kids to avoid dangerous play. This includes recklessness or goofing off. There are rules in sports for a reason. Learning correct technical form and building skills will make concussions and all types of injuries less likely to occur.
Injury 4: Little League Shoulder
For baseball or softball players, constant strain and stress on the shoulder from the excessive throwing of a ball causes microscopic damage to the growth plate, which results in pain and swelling. Gymnasts incur similar damage in their wrists and body as well. Repetitive training is a significant contributing factor. Little League shoulder is considered a growth plate injury.
How to Prevent Little League Shoulder
Don’t play one sport all throughout the year. Teens need at least three months away from a sport to allow microscopic damage, a.k.a. microdamage, to growth plates to heal. Changing up physical activity routines for a couple of months every year will work out other muscle groups.
Injury 5: Ankle Sprains
Sprained ankles are so common we all know at least one person who has suffered a sprain in their lifetime. Teenage athletes commonly deal with these. Ankle sprains occur when supporting ligaments of the ankle become torn or stretched past the point they’re supposed to stretch. You can get one from running on a field and inadvertently step on a pebble or in a hole. Ankle sprains fall into the category of acute injuries.
There are three types of ankle sprains. They are classified by severity of the injury:
- Grade One: This is the least severe level of injury. Ligaments stretch just slightly. The pain felt in a Grade One sprain presents with a little soreness and perhaps a small amount of swelling.
- Grade Two: The ligaments tear, but just a small part of them. This painful sprain will remain swollen. You will be hard-pressed to put weight on your foot with a Grade Two ankle sprain.
- Grade Three: The most severe sprain, Grade Three means the ligament is completely torn. This type of sprain is incredibly painful and produces formidable swelling. Attempting to put weight on this sprain will be nearly impossible because of the severity of the injury.
How to Prevent Ankle Sprains
Instruct your teen to never skip a chance to warm up and stretch. Tell them to always do this before working out or participating in competitive sports or miscellaneous physical activity.
Teach teens to look where they walk. It sounds simple enough, but it really helps to be aware of upcoming steps. Advise them to look for surfaces that aren’t level and for cracks in the sidewalk or asphalt. They should also look out for twigs and rocks. Stepping on one of these unaware can cause ankle sprains.
Make sure teens get plenty of rest off the field. Fatigue leads to sloppiness, which ups the chances of getting injured. If they are tired, remind them to add extra vigilance and look at their surrounding walking and running surfaces. If your teen has weak ankles that sprain easily, utilize braces, tape or supportive shoes for added protection.
Injury 6: Jumper’s Knee
Jumper’s knee is when the kneecap tendon becomes injured or inflamed. The kneecap’s tendon, also known in medical terms as the “patellar tendon,” connects the kneecap to the bone in the shin. This injury is an example of overuse. Overuse refers to movements that repeat over and over, causing damage to tissue in specific parts of the body.
Basketball is a frequent culprit in jumper’s knee. In basketball, the athlete lands from jumps, switching directions suddenly, and shuffling up and down the court with countless stops and starts. All these movements contribute to jumper’s knee. They place a strain on the patellar tendon. Teens who routinely participate in volleyball, gymnastics and running place a lot of stress on their knees. Jumper’s knee is considered an overuse injury.
Common symptoms of jumper’s knee include:
- Pain that occurs below the kneecap
- Knee stiffness, especially during jumps, kneeling, walking up the stairs and squatting
- Pain when bending the knee
- Pain in the thigh muscle, or quadriceps
- Weakness in the calves or legs
How to Prevent Jumper’s Knee
Stretching is the most essential preventative for jumper’s knee. Prepare a routine for your teen to warm up and stretch out their quads, calf muscles, and hamstring muscles to head off potential injury. Set aside some extra time for your teen to stretch their legs after exerting themselves as well.
Injury 7: Quadriceps Contusions
The muscles on your leg located in the front of your thighs are called quadriceps. Quadriceps assist in flexing your hip. They also help to straighten your knees every time you run or walk. Quadriceps connect to the thighbone or femur. A straight-on hit to your thigh can give the muscle a violent shove right into the bone. When this happens, the injury can be pretty painful and severe. Quadriceps contusions are categorized as acute injuries.
You can get two types of quadriceps contusions. An intramuscular contusion occurs when a muscle becomes torn inside the lining that envelops it. An intermuscular contusion occurs when a tear happens in both the muscle and the lining that surrounds said muscle.
Teens who play sports like hockey, lacrosse, football and soccer are at an elevated risk of getting quadriceps contusions due to the constant collisions that occur in these sports. Quadriceps contusions are separated into three categories:
- Grade One: These are the least painful of the three categories. There’s a little bruising, a little pain and minor tenderness. If there is any swelling, it will be minimal. Walking isn’t hindered, nor is bending of the knee.
- Grade Two: These contusions present with more pervasive bruising. There is visible swelling and most likely quite a bit of trouble moving around. If you move, you’ll probably walk with a limp. The bruised area will be tender. Knee bending will be difficult.
- Grade Three: Contusions at Grade Three will be deep. A lot of swelling and pain will let you know you’re at Grade Three. Bending the knee will be very difficult, as will walking on your own. Knee bends will be very hard, as will attempts at straightening your injured leg.
How to Prevent Quadriceps Contusions
Invest in protective equipment that fits your teen well. When playing high-risk contact sports, make sure your child wears the required padded pants.
Remember the rules. Play by the rules of any sport, and there is a lesser chance of injury.
Tell teens to keep their physical limits in mind and exert themselves within their abilities. Knowing their limitations will decrease risks of injury. This mostly applies to recreational sports like snowboarding, skiing and skateboarding.
General Tips for Preventing Common Injuries in High School Athletes
Here are a few more injury avoidance tips for young athletes who play all kinds of sports:
- Get Adequate Sleep: Teens who don’t get enough sleep are more likely to be injured while playing sports. Teens who get at least eight hours of sleep every night have a 68% lower risk of sports injury compared to those who sleep less on a regular basis.
- Take a Day Off: Taking at least one day off from sports per week is beneficial. A young athlete’s body needs this time to recover.
- Take Breaks During Practice: Taking breaks during practice and games reduces the risk of getting injured. It will also help in fending off heat-related illnesses on the field during the warmer months.
- Stay Hydrated: Drink plenty of fluids before, during and after games and practices.
- Increase and Maintain Flexibility: Before exercise, practice or games, do some stretching. A little stretching goes a long way in preventing injuries.
Watching your young athlete play can be exhilarating and joyous. If an injury does happen, it is scary to see your child get hurt on the field. For compassionate, experienced orthopedic care and advice on how to help your high school athlete deal with an injury, contact Orthopedic Institute of Pennsylvania. We have treated kids in Central PA for injuries for years, and we can help you and your family through this difficult time.
Employee Summer Picnic!
Over the weekend, we celebrated our employees with our summer picnic at the Harrisburg Senators Game! It was an evening filled with food, fun, family, and friends! Check out some of the photos from the event!












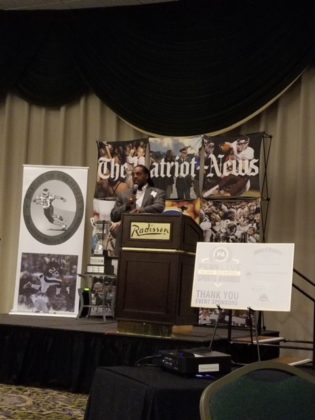
PennLive High School Sports Award Banquet
Last night, OIP was in attendance as a sponsor of the PennLive High School Sports Awards Banquet! Below we have some links to the action!
You can meet PennLive’s top boys and girls athletes in each high sport here: http://www.pennlive.com/sports/index.ssf/2018/05/meet_pennlives_top_boys_and_gi_1.html
The PennLive High School Sports Awards Photo Gallery is here: https://www.pennlive.com/expo/erry-2018/05/ec8366e77c5754/index.html
And, PennLive’s High School Sports Awards banquet red carpet video: http://www.pennlive.com/news/2018/05/pennlives_high_school_sports_a.html