How to Prevent Common Fall Sports Injuries
The roar of the crowd as the running back heads into the end zone for a touchdown. The satisfying smack of the ball as a middle blocker delivers a thundering spike. The sweet swish of a goal hitting the back of a soccer net. The unison cries of cheerleaders as they execute a cupie. The anguished yell of a player going down with an anterior cruciate ligament tear.
Those first four sounds are welcome signs that fall sports season has arrived. That last one is not, but alas, it happens all too often to athletes around the Central PA area. Fall sports injuries are commonplace, yet many of them are preventable when you plan ahead.
 This is important, because more kids than ever are playing sports. According to the National Federation of State High School Associations, an all-time-best 7.8 million kids participated in sports last year, including more than 319,000 in Pennsylvania. Many of their parents also remain active, with one in four still participating in sports.
This is important, because more kids than ever are playing sports. According to the National Federation of State High School Associations, an all-time-best 7.8 million kids participated in sports last year, including more than 319,000 in Pennsylvania. Many of their parents also remain active, with one in four still participating in sports.
With this in mind, we’ve put together a guide to fall sports safety and injury prevention, designed to address concerns we hear from our patients and their parents about how to enjoy a fun and healthy fall season. We love sports, and we want our patients to feel confident and secure as they participate in them. Follow these tips to keep playing hard this fall.
The Most Common Fall Sports

You can play most any sport in the fall — even baseball, once relegated to spring, has fall ball while basketball has indoor leagues in October and November. But some of the most popular traditional fall sports at the high school, college or adult level include:
- Football
- Field hockey
- Cross country
- Soccer
- Cheerleading
- Volleyball
- Tennis
- Golf
These sports all require a mix of cardiovascular training and strength to succeed, as well as precision. It’s not easy to hit a tiny ball onto the green or veer around mud puddles that pop up suddenly as you run a course. Unfortunately, each sport also carries some risk, whether it’s from whacking into an opposing team’s player, being thrown up in the air, or executing a forehand swing again and again.
The Most Common Fall Sports Injuries
 Each year, some 1.35 million children suffer injuries while playing sports. Of those, strains, sprains and fractures are the most common. We treat those here at OIP, along with many other conditions. Here’s a look at some of the sports injuries most likely to be sustained during the fall and a few things to look out for and keep in mind when dealing with these conditions.
Each year, some 1.35 million children suffer injuries while playing sports. Of those, strains, sprains and fractures are the most common. We treat those here at OIP, along with many other conditions. Here’s a look at some of the sports injuries most likely to be sustained during the fall and a few things to look out for and keep in mind when dealing with these conditions.
Fractures

Nearly every sport calls for rapid movement, and you often come into contact with other players. Anyone who’s ever watched a penalty corner in soccer knows how easy it is to get knocked around when you’re going for the ball. Add in sticks in field hockey, and it’s little wonder broken arms and legs can happen.
Fractures hurt a great deal. Though we tend to think of a broken arm or leg, you can suffer broken bones in anything from your fingers to your metatarsals in your feet. Not every fracture is the same, either. We see a range of different broken bones:
- Open fracture: A bone pokes through skin
- Comminuted fracture: A bone has been broken more than once
- Bowing fracture: A bone bends but doesn’t snap, a condition limited to children
- Complete fracture: A bone breaks in two
- Greenstick fracture: One side of the bone is cracked, but the other remains intact
Fractures require immediate treatment. Not all breaks will need a cast, but many will necessitate a long break from the field.
Strains
Muscle strains come from sudden movements, moving in a way the body isn’t used to or overuse. We often think of strains as the aches that dog weekend warriors, but an athlete in great shape can still sustain a strain. Football, soccer and field hockey players tend to suffer more back and leg strains, while tennis, golf and volleyball players are more prone to arm, elbow and neck strains.
Symptoms of a muscle strain may include:
- Swelling
- Spasming
- Cramping
- Trouble moving
The best treatment for strains includes a mix of rest, icing and elevation. Your muscle needs time to repair itself, which will happen more quickly if you reduce the pressure on it by letting it relax as much as possible. For a leg or ankle strain, crutches may even be necessary for a few days. In severe cases, surgery could be necessary for a strain, but most will heal in a short period of time.
Sprains
Sprains are tears or stretches of your ligaments, which tether bones together at a joint. Most sprains occur when you twist part of your body in an awkward way. For instance: you land on the side of your ankle instead of your foot after kicking a ball. Fall sports can lead to all types of sprains, from ankles to elbows and knees. Hand injuries can even occur in a sport such as soccer, where you don’t use your hands, if you fall and land awkwardly on your hand.
Many people who tear their ACLs, one of the most devastating types of fall sports sprains, often report hearing a pop or feeling the tear. An ACL injury may require surgery and months of rehabilitation, and athletes may be limited in what they can do on the field when they return. In most cases, however, you can heal from a sprain through:
- Rest
- Icing and compressing
- Immobilizing with a splint
- Elevating
- Taking anti-inflammatories to reduce swelling
Concussions
No matter the season, concussions are a constant when it comes to sports. Contact sports such as football often lead to hard blows to the head. In soccer, repeatedly heading the ball can result in a concussion. Cheerleaders can fall from heights of five feet or more when executing flips, lifts or pyramids. Not every blow to the head results in a concussion, but they can occur from what may appear to be a mild knock.
Be aware of the symptoms of concussions and keep an eye out for them after a head blow. They include:
- Nausea or vomiting
- Head and eye pain when exposed to a bright light
- Confusion or disorientation
- Fatigue
- Ringing in the ears
If you experience those symptoms, you should contact your doctor immediately. They’ll recommend the proper treatment, which will likely include a mixture of rest and refraining from activities that require a lot of thinking. If you’ve had more than one concussion, you may need to discuss further safety measures to avoid long-term brain distress.
Shin Splints

Do your lower legs feel sore or tender? Does it hurt when you run? You may have developed shin splints, an overuse injury often seen in fall sports where athletes run at a high intensity, such as cross country, soccer or field hockey. The repetitive motion of running — jarring the tissues holding your muscles to your bone — causes shin splints.
They tend to occur early in a season, when your body isn’t used to running, and ease as your body adjusts. Upping your mileage or workout intensity too quickly can spur shin splints, as can running on hard surfaces, such as concrete. You may be predisposed to developing shin splints if you have high arches, too.
Most cases of shin splints will respond to the usual treatments for strain, including rest and icing. It’s important to take time away from your sport to allow your body to heal sufficiently before you start running again. But in a small number of cases, athletes need further treatment, such as:
- When the orthopedist suspects a stress fracture
- Tendonitis develops
- You don’t have shin splints at all, but rather a rare condition called chronic exertional compartment syndrome, in which pressure builds up in the muscles.
Patellofemoral Syndrome
Pain in the front of the knee can be excruciating. If your knee hurts when you squat, sit, walk up the stairs or jump, you may have developed patellofemoral syndrome, which is common in athletes, and especially in teens. Symptoms include the knee buckling or making grinding and popping sounds.
Patellofemoral syndrome occurs when the cartilage beneath the kneecap becomes worn or soft. This can lead to a shifting of position of the kneecap, and poor alignment can cause the pain.
Initially, your doctor will advise you to avoid any activities that cause pain in the knee. It’s also treated by:
- Wearing a brace to keep the kneecap in place
- Ice and rest
- Avoiding long periods in bent-knee positions
- Strengthening the knee with stationary bike riding
- Taking an anti-inflammatory medicine
How to Prevent Fall Sports Injuries
Now you know what injuries fall sports players are most susceptible to. The good news is, you may be able to avoid some of these injuries.
 The first and most important rule of injury prevention for any sport, whether it’s football or field hockey, is to get a physical. Most high schools and middle schools require athletes to have a physical at the beginning of any sports season. The pediatrician will examine the athlete for any signs they should not be competing, or tip off parents for things to keep an eye on.
The first and most important rule of injury prevention for any sport, whether it’s football or field hockey, is to get a physical. Most high schools and middle schools require athletes to have a physical at the beginning of any sports season. The pediatrician will examine the athlete for any signs they should not be competing, or tip off parents for things to keep an eye on.
The physical is essentially a proactive way to address any limitations or problems your child may experience in their chosen sport. For instance, if a volleyball player suffered an ACL tear a year earlier, the doctor may have special instructions about running and jumping. You may also want to consult your child’s orthopedist if they’ve had issues in the past.
Of course, not all athletes are kids. In fact, injuries can be far more common for “weekend warriors” who limit their activity to short, intense bursts on the weekend. They put themselves at greater risk of getting hurt because their body has not been conditioned to such intensity. It’s easier for a muscle to tear or an ankle to give out when the body is put in such distress.
If you haven’t had a physical in a couple years — or worse, longer than that — get to the doctor before your flag football, soccer or volleyball season begins. Think of it like your yearly car inspection. You need to know everything’s working right before you can get back on the road.
Other Fall Sports Safety Tips
If you or your child have already had your physical, great job! But there are a number of other fall sports injury prevention tips you can follow. Make sure you keep these in mind so your family can enjoy a fun and injury-free season.
Warm Up Properly
Tip: Getting the body limber and ready to move will prevent many sports injuries. To reference the car analogy once more, your car can’t go from 0 to 100 miles per hour in an instant. It needs time to build to that top speed. It’s the same for your body.
 Execution: Perform stretches and light calisthenics before any game or practice instead of jumping into sprints or full-body blocking, and your body will be ready to move without hesitation.
Execution: Perform stretches and light calisthenics before any game or practice instead of jumping into sprints or full-body blocking, and your body will be ready to move without hesitation.
Cross-Train to Prevent Injury

Tip: The stronger your body is, the better it can handle strains and respond to pressure. Many athletes these days have a tendency to specialize — that is, to play just one sport. That can be great for developing skills, but it means your body does the same thing over and over, and it can make you more susceptible to injury. Challenging the body with new exercises, including weight-bearing exercises that strengthen bones as well as muscles, will help you improve as an athlete, too.
Execution: At least once a week, do something other than your chosen sport. If you’re a runner, try lifting weights. If you’re a football player, try swimming. If you’re a volleyball player, try biking. Use different muscles in order to balance out your regular training.
Make Sure Courts and Fields Are in Good Condition
Tip: You wouldn’t let your child go to a school where the doors were falling off their hinges or the windows were bashed out. Don’t let them play on a shoddy field or court, either — the consequences can be just as dangerous. If a soccer player streaking down the field suddenly catches their foot in a divot, they could sprain their ankle or worse.
Execution: Ask coaches if playing surfaces have been inspected. Don’t be afraid to speak up. If this concern has never been raised before, offer to act as a liaison between your league and others to improve the condition of area fields. For youth and adult sports, many leagues rely on volunteers to get fields ship-shape. You may need to help out to ensure your or your child’s safety.
Rest After Sustaining an Injury
Tip: Athletes tend to be competitive. They want to get back on the field as soon as possible, and many will try to skimp on the time off they’ve been told to take. They may claim “I feel fine!” or “I don’t really need three weeks of rest!” But that’s usually not true. The doctor has prescribed this time off because it’s necessary to heal properly, even if they can’t feel it happening.
Execution: Follow doctor’s orders to the letter. Don’t return to the field until the doctor has okayed it. Though it may seem devastating to miss a “big game,” athletes who come back too soon could be endangering their careers, not just their seasons.
Speak Up About Pain
Tip: Especially when you’ve suffered a blow to the head, being proactive can help protect your health. Concussions carry even more serious consequences when they are not treated. There’s often a desire among athletes to appear “tough,” so they play through the pain. But in truth, pain is your body’s way of telling you something’s wrong.
Execution: See your doctor or orthopedist if you suffer pain that lasts more than a few hours, you suffered a blow to the head or you simply know something in your body isn’t right. Remember: the sooner an injury gets treated, the sooner you can be back on the field.
Invest in High-Quality Equipment
Tip: Playing sports can be expensive. It’s tempting to skimp on some of the “extras,” such as mouth guards or cleats, that aren’t provided by the school or that you have to replace every few years. But in the long run, it’s better for your wallet — and your health — to spend the money on proper equipment to keep you or your child safe.
Execution: Talk to other parents or your teammates about where to find the best-quality equipment. A coach or trainer may also recommend effective brands or stores. You can often find dentists or dentists-in-training who will outfit teams with mouth guards for free, as a public service.
Change Positions
Tip: When you play the same position in every game and practice, you repeat the same movements day after day. This repetitive motion leads to bursitis, or inflamed bursa sacs, and tendonitis, or inflamed tendons. Though getting reps at the position you play is important, you should also be moving around the field to prevent these repetitive motion injuries.
Execution: This can even benefit your team, if you need to build an argument to an overzealous coach. It helps the quarterback of a football team to understand what their receivers see on the field. This will help him get the ball to them more effectively if he understands, for example, where to throw the ball to keep it away from a defensive back who’s closing in.
Enjoy Downtime
Tip: Playing sports is fun. You may want to do it year-round, month after month. But your body needs a break. Instead of going from football to basketball to baseball, make sure you take some time off between seasons. In addition to allowing your body to rest, it helps avoid mental burnout, which can lead to injury when you become too tired to use proper form or pay attention during key moments of a game.
Execution: Even just a week’s break between your fall and winter sport can give the body some much-needed downtime. Go see movies, plan a vacation or veg on the couch. Being inactive for a few days can be just as valuable as being active the rest of the year.
Fuel Your Body Properly
Tip: A strong body will resist injury better than a weak one. Eat a balanced diet with lots of calcium to build strong bones that keep you running fast. Hydration can also be tricky during the fall, often leading to dehydration and poor form that encourages injuries. Fall’s early months can be just as hot as the summer, so don’t skimp on water during practice and games just because the calendar says it’s late September. And don’t forget to stay hydrated during the chilly month of November, even though you may be sweating less than you did two months ago.
Execution: Drink before, during and after your game or practice. Try new veggies and fruits every week to keep your diet interesting. Find tasty sources of calcium to provide insurance for your bone health.
Have You or Your Child Sustained a Fall Sports Injury?
Sometimes, despite your best precautionary efforts, injuries happen. We’re here to help you get through them. If you or your child gets injured during a fall sports game or practice, contact OIP. We can help diagnose the problem quickly and work to have you or your child back in the game — after the proper amount of rest, of course.
Clearing the Smoke Around Joint Replacement
Did you know the risks of complications after a total joint replacement are increased for smokers?
- The infection rate is six times higher in smokers than in non-smokers.
- The rate of blood clots and wound complications is significantly higher in smokers.
However, If you stop smoking four weeks before joint replacement surgery, you can reduce your risk of complications by 41%! On average, each week you are able to avoid tobacco; your risk of complications goes down by 19%. If you eliminate nicotine, the blood flow to your skin returns to normal in two weeks, allowing more normal surgical wound healing.
If you are also able to avoid smoking for two weeks after surgery, your wound healing complications are significantly reduced. In addition, some prostheses are not cemented into place. For long-lasting success, they require your own bone to grow into the prostheses. That would require at least six months of smoking cessation after surgery to optimize your chance of a successful joint replacement.
If you decide that stopping smoking is the right thing for you to do, up to 22 percent of people who stop in order to undergo a joint replacement never go back to smoking.
So if you are considering a joint replacement surgery, please seriously consider stopping smoking four weeks before surgery and do not smoke at least two weeks after surgery. You can consult with your orthopedic surgeon and your primary care provider for ideas and options for smoking cessation.
What You Need to Know About Anterior Hip Replacement Surgery
– Differences Between Posterior and Anterior Hip Replacement Surgery
– Preparing for Anterior Hip Replacement Surgery
– Recovery After Anterior Hip Replacement Surgery
Conditions That Can Lead to Hip Replacement Surgery
While Roger’s pain started immediately after a near spill on a slippery, sandy beach, his doctor explained that he had an underlying issue that would have made hip replacement surgery inevitable at some point of his life. Common conditions that often lead people to have either posterior or anterior hip replacement surgery include the following:
- Osteoarthritis
- Rheumatoid Arthritis
- Osteonecrosis, also known as Avascular Necrosis
- Injury
- Fracture
- Bone Tumors
For most people, hip pain starts as a minor discomfort and worsens over time as their hip joint continues to deteriorate. Depending on the amount of pain you’re experiencing and how your damaged hip joint is impairing your ability to do routine things, your doctor may initially choose to treat your hip without surgery to delay the procedure for as long as possible. Alternative treatments include the following:
- Exercise: An exercise regimen can strengthen the muscles around your hip, which can alleviate your pain and make it easier for you to perform the tasks that are part of your daily routine.
- Walking Aids: Walking aids such as a cane or walker can relieve some of the stress on your hip, which can help you postpone hip replacement surgery.
- Acetaminophen: If you have hip pain without inflammation, your doctor may use this medicine to control your pain.
- NSAIDs: If you have hip pain with inflammation, your physician may treat your pain with a nonsteroidal anti-inflammatory drug such as aspirin or ibuprofen.
- Topical Treatment: Some people treat their hip pain by applying a topical analgesic product on the skin around their hip.
- Corticosteroid Medications: When NSAIDs fail to reduce a patient’s hip pain, the individual’s doctor may try to delay hip replacement surgery by prescribing corticosteroid medications such as prednisone or cortisone to alleviate the person’s discomfort. Depending on your doctor, they may inject a corticosteroid directly into your hip joint.
Deciding to have hip replacement surgery is a very personal decision. You have to consider various factors, including your finances, health insurance, the length of your recovery, the ability of your friends and family members to help you as you recover and the amount of vacation and sick time you have at work, just to name a few. In general, the time may be right for you to consider hip replacement surgery if you’ve exhausted your alternative treatment options and your pain and loss of joint function have negatively impacted your quality of life.
Differences Between Posterior and Anterior Hip Replacement Surgery
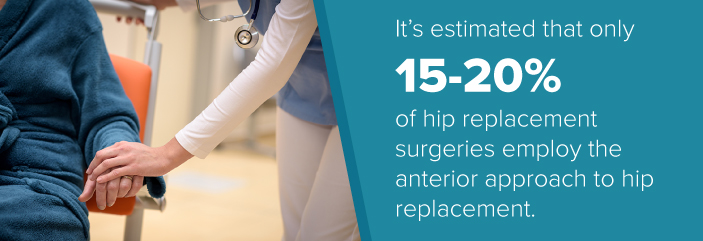
While many people seem to think that total hip replacement using an anterior approach is a new procedure, the truth is that doctors developed the anterior method of hip replacement surgery more than 50 years ago. The Centers for Disease Control and Prevention reports that surgeons perform approximately 332,000 total hip replacements in the United States each year, while the New York Times reported that around 400,000 total and partial hip replacements are performed in America annually.
According to the American Association of Hip and Knee Surgeons, the number of hip replacements performed annually may grow to 500,000 by 2030. Despite the frequency of these surgeries, it’s estimated that only 15-20 percent of hip replacement surgeries employ the anterior approach to hip replacement. However, that doesn’t mean one method is superior to another.
Even though surgeons have performed both posterior and anterior hip replacements for decades, anterior hip replacement surgery has only started to become more common as the medical world strives to provide patients with a more overall positive experience. There are many reasons why more posterior hip replacement procedures are performed, but the two most likely factors are the specialized training and equipment that are typically necessary to conduct anterior hip replacement surgery successfully.
Each approach has unique benefits and risks, which your orthopedic surgeon will discuss with you fully ahead of time. However, in addition to the training and equipment required by those performing the anterior technique, there are some distinct differences.
Both procedures involve removing the damaged head of the femur and any damaged cartilage from the socket. Then, a metal or ceramic ball is attached to the bone, and a new metal socket is put in place. Between the new ball and socket, a plastic spacer allows for a smooth gliding movement. But there are several aspects of these two methods that distinguish each approach to hip replacement surgery from the other:
- Entry Point: In posterior hip replacement surgery, a surgeon will make an incision on the outer buttocks at the back of a patient’s hip or on the side of the person’s hip which is usually ten to twelve inches long. With anterior hip replacement surgery, an incision is made on the front of a person’s hip and is four to five inches long.
- Muscle Detachment: With the posterior approach to hip replacement, a surgeon has to cut through major muscles to access a patient’s hip. Since there are fewer muscles in the front of a person’s hip, a surgeon can work through muscle fibers while performing anterior hip replacement surgery instead of having to cut through them.
- Hospital Stay: With a posterior hip replacement, patients can expect to stay in the hospital for three to ten days. The anterior approach, however, allows them to return home within two to four days.
- Recovery Time: Because the posterior technique involves cutting muscles around the hip joint and giving them enough time to repair, the recovery time is longer — generally two to four months. Since the muscles around the hip joint are not cut with the anterior approach, recovery only takes two to eight weeks.
- Post-Surgical Precautions: When patients undergo a posterior hip replacement, they must follow a set list of very careful precautions for up to 12 weeks to prevent further injury. Because the anterior approach has less risk of complications, there are no specific precautions that need to be followed.
As we mentioned, the posterior method is the approach most commonly utilized by orthopedic surgeons because many believe it gives them better visibility of the joint. They also feel it provides for more precise placement of hip implants. In many ways, the posterior approach is minimally invasive, but the anterior technique is even less invasive.
As the medical world revisits what makes a successful hip replacement, there are those who embrace the anterior approach as a better method of total hip replacement. The actual amount of time spent in surgery is shortened using this technique. It also allows for patients to recover faster, regaining mobility quickly with minimal pain. And many feel that it minimizes the risk of complications for the patient before, during and after the operation.
Even though posterior hip replacement surgery and the anterior approach to hip replacement differ in several key ways, the goal of both procedures is the same. Both surgeries are designed to alleviate anterior hip pain and restore function so that people can resume their normal daily activities without experiencing discomfort, or at least without as much discomfort as they had before surgery.

According to one source, experts consider total hip replacement surgery “among the most valued developments in the history of orthopedics” regardless of which method is used to restore a person’s mobility and reduce the individual’s pain. Hip replacement surgery doesn’t just provide short-term benefits, it also provides lasting ones. According to some studies of knee and hip replacements, 90 percent of artificial hips still function after 20 years and 70 percent of the manufactured joints still work after three decades.
No matter which approach is chosen, the hip joint has one of the highest success rates for recovery after a surgical replacement. The most important factor is not whether to pick posterior or anterior, but the experience and reputation of your surgeon. An experienced doctor will ensure your risk of complications is very low. The team at OIP is well-known in the field of orthopedics both in Pennsylvania and beyond, and we’re here to ensure you have all the info you need to make an informed decision.
Benefits of the Anterior Approach to Hip Replacement
Anterior and the traditional posterior total hip replacements both have excellent outcomes. The real advancement in total hip replacements that has improved patient recovery is the rapid rehabilitation following both types of approaches. Patients are out of bed within 2 hours of surgery and are frequently home within 24 hours of surgery. Exercises learned pre-operatively are started immediately post-operatively, and recovery can be quite rapid. Patients are treated like athletes and not like patients!
However, the anterior approach does seem to have some additional benefits that many patients enjoy when they choose this method of hip replacement. This includes:
- Less Major Muscle Damage: Because the anterior approach avoids cutting through muscle, this allows for less damage to occur as a result of the surgery. It also means surgeons don’t have to make repairs to these muscles once the operation is complete.
- Less Pain: Patients typically don’t experience as much pain because the surgeon doesn’t have to cut through muscle.
- Quicker Recovery: After the surgery is complete, patients are encouraged to move and bear weight as soon as it’s comfortable. This is often not possible with posterior hip replacements.
- Decreased Risk of Hip Dislocation: The muscles and soft tissue around the hip naturally prevent it from dislocating. When these are cut, as with the posterior method, there is a greater risk of hip dislocation. The anterior technique avoids this by not cutting into the muscle.
- Improved Range of Motion Sooner: With the posterior method, patients have to avoid bending at the hip, internal hip rotations and even sitting with their legs crossed for six to eight weeks as this could cause a hip dislocation. However, the anterior method does not place these prohibitions on patients.
Although there are many benefits to having anterior hip replacement surgery, you should be aware of some precautions before you decide to have anterior hip replacement surgery instead of a posterior hip replacement. These include:
- Not for Everyone: Unfortunately, not everyone is a candidate to have an anterior hip replacement even if they need to have a hip replaced. Anterior hip replacement is generally not an option for people who are obese or extremely muscular, for instance, because they have additional soft tissue that can make it hard for a surgeon to access the patient’s hip joint.
- Possible Nerve Damage: One of the anterior hip replacement complications that can arise is possible nerve damage. It’s important to note that nerve damage is also possible if you have a posterior hip replacement. If nerve damage occurs, you may experience numbness in your thigh. While it happens in less than one percent of patients, nerve damage can also cause meralgia paresthetics, which is an irritation of the skin that the damaged nerve supplies.
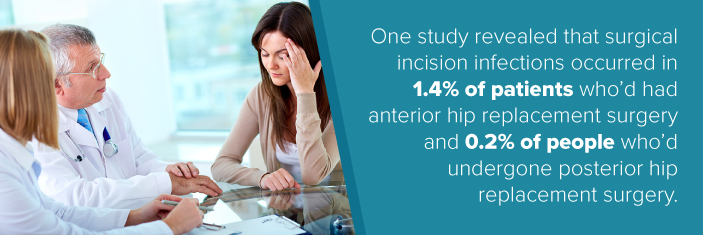
- Problems With Healing: One of the anterior hip replacement precautions you should know about is that your incision can become irritated if it’s not cared for properly. One study revealed that surgical incision infections occurred in 1.4 percent of patients who’d had anterior hip replacement surgery and 0.2 percent of people who’d undergone posterior hip replacement surgery. This type of mild complication normally resolves itself even if it’s left untreated by a doctor.
Preparing for Anterior Hip Replacement Surgery
“I found a lot of what I did before my surgery was very helpful during my recovery from anterior hip replacement,” said Roger B. “Probably the most important thing I did was get in shape. I’ve always tried to incorporate physical activity into my daily routine, but I made it a point to visit the gym more often than I normally did in the weeks and months leading up to my surgery. I also increased the length of my walks through the neighborhood as much as I could given the pain I was in.”
“I was 72 years old when I had my anterior hip replacement surgery and my kids were grown-ups. My orthopedic surgeon had advised me to arrange for someone to help me since I wouldn’t be able to drive or do certain things around the house for several weeks after my procedure. So, I called one of my daughters who agreed to help me out. Knowing my daughter was going to stay with me took a lot of pressure off when it came to taking care of everything else I needed to get done to prepare for my surgery. It also helped that she arrived in town several days before my operation and was able to help with my last minute preparations.”
While Roger’s daughter was able to help him throughout his recovery, not everyone has friends and family members whose schedules are flexible enough for them to help consistently during a patient’s anterior hip replacement recovery. If you can’t arrange for someone to stay with you, ask your doctor if it’s possible for you to stay in a rehabilitation center while you recover from your surgery.
In addition to making arrangements for your post-operative care and getting in better shape, there are other things you can do to prepare for your anterior hip replacement surgery, including the following:
- Prepare Meals: You can prepare meals that you can freeze before you go into the hospital to minimize the amount of cooking you or your caregiver will need to do in the days immediately following your operation. Potpies, lasagna, baked ziti and certain soups are all freezable options. You can store your food in single serving containers that can be warmed in your microwave with ease, or you can use freezer storage bags to store your meals.

- Rearrange Your Home: Since you’ll probably have to use crutches or a walker after your surgery, it’s critical that you remove any obstacles that may cause you to fall or that will impede your ability to move around your living space prior to your anterior hip replacement. If you have area rugs that may be tripping hazards, remove them. If a decorative table or another piece of furniture constricts a hallway, temporarily relocate the piece to a room that you won’t have to use during your recovery. Borrowing a walker from your doctor’s office and using it to navigate your home before your surgery will help you to identify the things you need to move.
If you have a multi-story home and your bedroom is not on the ground floor, you’ll need to create a sleeping space on the first floor because you will not be able to climb stairs immediately after your surgery. If it’s not practical for you to relocate your current bed because you have a spouse who also needs a place to sleep, consider relocating one from a spare bedroom, buying or renting a hospital bed.
Move the things you’re going to use most often to the place where you’re going to spend most of your recovery time. Make sure your telephone, computer, remote controls and e-reader will be within reach from the seat you’ll be in for the majority of your recovery period. Make sure you have a bell or another device that you can reach easily to alert your caregiver in the event you need emergent or immediate assistance as well.
These steps will help you prepare for your surgery:
- Get the Tools You’ll Need: Depending on the hospital where you’re going to have your surgery performed and your health insurance, staff may provide you with some helpful tools before you’re discharged. These things include items such as reachers, a portable urinal, a raised toilet seat and a shoehorn that has an extra-long handle. Ask your doctor if you’ll be given these things after your anterior hip replacement. If not, ask him or her which items you’re likely to need, inquire about where you can get them and purchase them prior to your procedure.
- Make an Appointment with Your Physical Therapist: By visiting your physical therapist before your operation, you can learn exercises that can help physically prepare you for your surgery. You can also become familiar with the exercises you can do after anterior hip replacement. If you practice these moves beforehand, they’ll be easier for you to do after your surgery.
- Review Your Legal Documents: Certain risks are inherent in any surgical procedure. While anterior hip replacement surgery is not as invasive or life-threatening as many other operations, things can still go wrong. To make sure you’re prepared for any contingency, you should take some time to ensure your affairs are in order prior to having your operation. Review your will and living will. Make sure someone is legally authorized to make decisions on your behalf if you’re unable to do so yourself. Be sure to clearly communicate your wishes to your loved ones and your power of attorney. Doing so will make any decisions they may have to make easier on them.
Anterior Hip Replacement Surgery Recovery

As the less invasive approach to total hip replacement surgery, the anterior technique allows for a shorter recovery and rehabilitation time. This means patients can return to daily activities and even go back to work sooner. However, the recovery process still involves distinct phases to ensure the tissue is healing properly and that you will have maximum functionality.
Although each patient is different, there are a few things you can anticipate during the recovery process after anterior hip replacement surgery. However, your progression depends totally on your unique set of circumstances. One of the greatest advantages about recovering from an anterior approach to hip replacement as opposed to the posterior is that you won’t have to follow any specific anterior hip replacement precautions like not bending past 90 degrees or crossing your leg. This is because there is less risk of dislocation and less leg length discrepancy with the anterior technique.
After undergoing an anterior hip replacement surgery, here are some of the phases of the recovery process you can expect:
- Hospitalization: Patients undergoing the anterior approach usually only stay in the hospital for two to four days. During that time, the patient may receive their initial visit from a physical or occupational therapist. They may even encourage you to stand or walk a few steps using a walker or crutches. Movement after surgery is essential as it increases blood flow and reduces the risk of blood clots.
- Physical Therapy: Formal physical therapy will start shortly after your hospitalization. The goal is to improve muscle strength as well as increase range of motion and mobility. A unique program of exercises will be formulated to meet your specific needs. Therapists will consider any movement restrictions you have as well, so you have the safest possible recovery.

During the antererior hip replacement recovery time, your doctor and your physical therapist will work together to ensure you are on track for a successful recovery. They will be looking out to make sure you reacquire full balance, your tendons and muscles stretch properly and your muscles regain their full strength.
At first, you will have to use a cane or walker to get around. However, unlike the posterior approach, there should be less post-operative pain. In fact, many are able to bend at the waist and put weight on their leg not long after the surgery is complete. This means those who undergo an anterior hip replacement can use a cane or walker sooner. Some patients require the use of pain medication.
After a few weeks of physical therapy, most patients are able to return to functional mobility, moving freely and going about their everyday tasks. A few weeks after that, you should be able to enjoy recreational activities as well. Just remember that everyone is different, and your doctor and physical therapist will be your guide during this process. Some patients take longer to recover fully, and that’s completely okay.
By the time you reach full recovery, there should be little to no pain, especially compared to the discomfort experienced before your surgery. And you should also be able to return to full normal function. There is a risk that the hip will be less flexible than a natural hip. For example, sitting cross-legged on the floor or even simple tasks like putting on your shoes and socks may be more difficult. That’s why it’s important to continue exercising and flexibility training even after physical therapy is complete. Low-impact aerobic exercises, like swimming, biking or walking, will help keep hip muscles strong and flexible.
WHY CHOOSE THE ORTHOPEDIC INSTITUTE OF PENNSYLVANIA

If you have hip pain or you’ve lost some function in one or both of your hips, contact the Orthopedic Institute of Pennsylvania to make an appointment today. We know you have many choices when it comes to orthopedic care, which is why we’re committed to making a difference in your life by going above and beyond your expectations every day. We promise to be part of the solution to whatever health problems you’re currently having and we’ll stand by you and support you as we work through them together.
We’ve improved the lives of other people who lived with pain and the loss of joint function too long, sometimes for years, and we can do the same for you. Don’t just take our word for it, though. Read what some of our patients had to say about their experiences with us:
“I can’t thank you enough for the new life you have given me. I have not been this happy in years.” – OIP Patient
“Dr Lippe was excellent in my care! From the first time I met him, to my surgeries, he was outstanding! Dr Lippe gave me my quality of life back! I will never be able to thank him enough! The pain I was experiencing was ruining my life! But Dr Lippe and his staff were all excellent in my care!” – Patricia C.
“Dr. Frankeny has absolutely given me my life back. It has been six weeks and I am feeling great. I barely use my cane. After enduring pain for over a year and [being] barely able to walk, I cannot believe my good fortune.” – OIP Patient
You don’t have to live with hip pain or be limited by a bad hip any longer. Schedule an appointment with the Orthopedic Institute of Pennsylvania to learn what we can do for you and see why our patients love us so much. We’re excited to be part of your solution.
Stories From Our Patients
Roger B. was a police officer for nearly thirty years before he underwent double knee replacement surgery in the late 1990s. “I knew I needed to have my knees done for years before I actually had the surgery. Even though it was painful to do my normal daily activities, I had to postpone the surgery for as long as I could because my wife had suffered a series of devastating strokes and needed my help on the home front. When I realized I couldn’t tend to her the way I needed to, that’s when I knew I couldn’t put the surgery off anymore.”
“After my wife died several years ago, I resumed fishing and some of the other things I wasn’t able to do during the years leading up to her death. On one fishing trip, I stumbled on the beach and ended up twisting in a way that wasn’t natural. From that point on, I had never-ending pain in my right hip. I tried, in vain, to reduce the pain by changing the way I walked, taking over-the counter pain medication, getting shots in my hip joint, etc., but nothing helped. When I realized I couldn’t pick up my granddaughter anymore because of the pain and I couldn’t sleep for more than an hour or two at a time because of my discomfort, I knew I had to do something.”
“Living in a retirement community, I knew a lot of people who’d had hip replacement surgery due to anterior hip pain. What I didn’t realize, however, was that there were two kinds of total hip replacement surgeries, posterior and anterior hip replacement surgery. The more I learned about the two procedures and the more I thought about what I saw during my neighbors’ differing recovery times and experiences, the more I started to think that the anterior approach was right for me.”
“So, I started to look for an orthopedic surgeon who was familiar with the procedure. I met with several doctors before I found one who was experienced with anterior total hip replacement surgery. Given my doctor’s extended experience with hip replacement and the anterior approach, I decided to go through with the procedure. Moreover, I’ve got to tell you, I’m glad I did. It gave me my life back and it did so a lot faster than I thought it would.”
17th Annual Dauphin County 50plus Expo

OIP is very excited to be participating again as a Sponsor and Exhibitor of the 17th Annual Dauphin County 50plus Expo, held at the Hershey Lodge, 325 University Drive, Hershey, PA, on Tuesday, May 31st, from 9:00 am – 2:00 pm.
Please stop by our booth (152-153) and say “hi!.”
Free Health Screening: OIP will be providing Heel Scans for Bone Density.
Door Prize: Be sure to register for a chance to win our door prize! We are giving away an OIP branded gift basket including OIP Apparel, Gift Card, and First Aid Kit.
Exhibitor Map and Listing: Download a copy of the Exhibitor Map and Exhibitor Listing in PDF.
For more information about the Dauphin County 50plus EXPO, visit www.50plusexpopa.com.
OIP Tops Patient Satisfaction Scores!
OIP voluntarily participates in a national patient satisfaction survey distributed by Talksoft / MedStatix.
We are proud to say that our results in the first quarter exceed the national standards in:
- “Staff works together well.”
- “Patients receive respect by scheduling staff.”
- “My privacy is respected.”
- “The doctors clearly explained procedures.”
“2015 Top Performers”
Four of our doctors received “2015 Top Performer” results in this national survey.
We are proud of Doctors:
- Steven B. Wolf, M.D.
- William W. DeMuth, M.D., F.A.C.S.
- Brett A. Himmelwright, D.O.
- John R. Frankeny, M.D.
Avoid Common Winter Injuries With These Helpful Tips
 If you’ve experienced an injury or pain while performing a wintertime activity, you are not alone. Personal injury during winter is likely to occur from performing simple activities, especially if you aren’t prepared to prevent an incident. From your back, shoulder and neck to joints and knees, pain and injury in these areas are commonplace during the winter.
If you’ve experienced an injury or pain while performing a wintertime activity, you are not alone. Personal injury during winter is likely to occur from performing simple activities, especially if you aren’t prepared to prevent an incident. From your back, shoulder and neck to joints and knees, pain and injury in these areas are commonplace during the winter.
The good news? Preventing winter injuries is possible, and you can enjoy the season without unnecessary pain and stiffness. Read on to discover information about winter back injuries, winter shoulder injuries, and — most importantly — health and safety tips to avoid any orthopedic winter injuries.
What Are the Most Common Winter Injuries?
Winter weather conditions bring with them a variety of potential risks for personal injury, as well as injury to others. Some of the most common winter incidents that lead to personal injury include:
- Falling on ice and snow
- Experiencing muscle strain from shoveling snow or scraping ice off the car
- Driving and motor vehicle collisions
- Accidents while playing winter sports and activities
Not all incidents will cause severe injury, but some winter accidents can be quite serious, especially for certain age groups and for people suffering from previous injuries.
Slipping and Falling on Ice and Snow
Slipping and falling on ice can be a scary experience. Ice can be difficult to see both at night and during the day. What looks like water pooled on the pavement can actually be a sheet of ice. You could step off the curb and right onto a slippery ice patch. When this happens, severe injury can occur if you fall to the ground. You may be able to recover and only skid briefly, but even if you don’t end up falling, you can wrench your back or experience another kind of injury in your attempt to recover.
Anyone is in danger of injuring themselves by falling or slipping on ice or snow, but seniors are especially at risk. In fact, according to the CDC, falls are the leading cause of injury among older Americans, and winter weather conditions only exacerbate that concern.
There are a variety of potential injuries that can occur from falls on ice, but the most common include the following:
- Bruises
- Head or brain injuries, including concussions
- Ankle strains and twists, and other kinds of muscle sprains and ligament strains
- Broken bones, most commonly hip and wrist fractures
- Back injuries, including spinal compression fractures
- Injuries to the spinal cord
Prevention is always the best method to avoid a slip or fall on icy days, and there are a few things you can try to keep you and your family safer:
- Wear proper footwear made for icy and snowy conditions.
- Keep your stride shorter and avoid long steps.
- Slow things down — try not to rush or run outdoors.
- Keep de-icer or sand on hand for when things get slippery around your house.
- In case of injury, always have your cell phone handy.
- If you need to do outdoor chores, take your time and don’t hurry.
Unfortunately, even with the best preventative measures, accidents happen. Skeletal and muscular issues arise every winter when people fall on ice or snow. If the fall is serious, you may need to call 9-1-1 or go to the ER immediately.
However, some people are unaware that they have a severe injury. This may be because they don’t feel the effects of the fall immediately, or they believe their pain and discomfort will pass with time. Symptoms like pain or swelling should not be ignored, and it’s important to seek the advice of a medical professional to assess your condition.
At OIP, we offer patients a 24/7 walk-in injury clinic for orthopedic emergencies such as falling on ice. Often, the waits are less than what you’d experience at an emergency room, and you will be able to get the specialized care of an orthopedic doctor trained to treat musculoskeletal injuries. In many instances, patients who go to the ER receive recommendations for them to seek out orthopedic specialists after the fact.
If you experience an injury on the ice or snow, whether it’s from slipping and falling or from attempting to prevent a fall, make an appointment with a specialist at OIP as soon as possible to determine if there is a serious injury. They will also be able to offer an effective treatment plan that meets your individual needs.
Shoveling Snow

One of the most loathsome winter jobs is shoveling the driveway and sidewalk. It can take a long time and require a lot of physical exertion. The low temperatures make the task of shoveling snow even more unpleasant. The repetitive actions of twisting and lifting while shoveling can cause severe strain on the body. All it takes is one muscle to be pulled the wrong way for your back, neck or shoulders to seize up.
Snow shoveling can be a potentially risky duty that can cause severe injury. A national study found that over the course of eleven years, there was an average of 11,500 emergency room visits due to snow shoveling injuries. The most common injuries reported were soft tissue injuries mostly to the lower back region. Among the remaining injury reports, lacerations and fractures were also reported, including injuries to the hands, arms and head.
Driving and Collisions

Most of us must continue to work and carry on with our normal, everyday activities even in snowy winter weather conditions. But if you aren’t prepared for winter driving conditions and don’t take the proper safety precautions, you can put yourself and others at risk. A study found that over a period of ten years, there were over 445,000 people injured as a result of weather-related vehicle collisions. The winter weather brings with it all kinds of potentially hazardous road conditions, such as:
- Wet pavement
- Sleet and slush
- Full coverings of snow and ice
Falling or Colliding During Winter Activities
One of the most enjoyable parts of winter is the fun you and your family can have with all kinds of winter activities and sports. From ice hockey and skating to skiing and snowboarding, there are plenty of ways to stay active and have fun in the winter. For kids especially, sledding and tobogganing are some of the best childhood memories of their winter seasons.
These winter activities can be quite risky if you aren’t practicing safety. Falls and collisions in many winter activities can cause several forms of injury. Broken bones and stiff muscles and joints are some of the most frequently reported injuries when it comes to outdoor sports and activities. Running outdoors along the sidewalk or on trails can also pose safety risks if the pavement isn’t salted and the trails aren’t properly cleared.
Types of Winter Injuries
These incidents produce various types of injuries, which can range from mild and easily treatable to severe and long-term. Some of the resultant injuries from these winter accidents most commonly include:
- Head injuries
- Shoulder injuries
- Back injuries
- Neck pain and tension
- Knee joint pain and soreness
- Wrist sprains
- Elbow fractures and dislocation
- Ankle sprains and strains
- Hip fracture and soreness
Head Injuries
Head injuries occur during the winter as a result of any number of incidents. Most commonly, falling on ice and hitting your head on the pavement can lead to a potentially serious brain injury. If this occurs, it will need immediate treatment by a physician. A brain injury can be difficult to treat, and often the symptoms won’t be noticed until long after the injury has occurred.
Head injuries can occur during winter activities like tobogganing, snowboarding and skiing, or one can also occur as a result of a motor vehicle collision, which has the potential to lead to serious long-term health consequences.
Shoulder Injuries
Shoulder injuries commonly occur when you fall on icy pavement. When your shoulder meets contact with the hard ice-covered pavement, dislocation can occur. This damage to the shoulder joint can be quite severe and leave you suffering from soreness and bruising for a long time afterward.
A torn rotator cuff can happen as the result of repetitive overhead motions from winter sports or shoveling snow. This muscle tear can leave you feeling sore and stiff and may result in a chronic injury as well.
Back Injuries
There are plenty of winter incidents and activities that can cause a back injury. The most common injury associated with shoveling snow is to the back, specifically the lower back. Back injuries can also be the result of a serious fall on the icy pavement or on the stairs. Falls during winter sports and activities can also result in a back injury.
Another common way to injure your back during the winter time is by scraping your car’s windshield to remove ice and snow. The bending and leaning motion your body performs while reaching across to scrape the ice can result in pulled and strained back muscles.
Depending on the level of severity, treating a back injury with heat may help to relax sore muscles. An injury that is caused by a fall on ice may damage your spine, so treatment by a physician will be required.
Neck Injuries
Like back and shoulder injuries, neck injuries can occur due to a number of different winter incidents. The repetitive motion of shoveling snow can certainly lead to stiffness and soreness in the neck muscles. Neck injuries can also happen when scraping snow and ice from your car’s windshield when your muscles become strained from leaning and reaching.
These injuries can usually be treated with a heating pad to relax tense neck muscles. If a neck injury is caused by a fall or a motor vehicle collision, it should be treated at the emergency room.
Knee Pain and Strain
High-impact winter sports can be very damaging to your knees over a period of time. This type of injury usually occurs while performing activities and sports such as skiing and snowboarding, where your knees are absorbing the shock of hard landings. Running outdoors on pavement can also cause a similar injury to your knees. The best thing to do with a knee injury is to take it easy until it heals, avoiding any high-impact activities.
Wrist Fractures and Strains
A fall on the icy pavement can cause wrist injuries such as fractures and strains. When you take a fall, your natural instinct is to extend your arms and brace your fall with your hands. The impact of the fall on your hands can cause a severe wrist strain or even fracture.
The result can be a serious injury if not treated properly. Your wrist may heal improperly, which could lead to chronic pain later in life.
Elbow Injuries
Like wrist injuries, elbow injuries can also arise from a fall on icy pavement. When you extend your arms to brace your fall, not only do your wrists take the impact but your elbows do as well. Your elbow could become dislocated if the impact is so significant that it pops your bone out of position. Otherwise, a more potentially severe injury could be an elbow fracture. This can lead to long-term pain if not treated properly.
Ankle Strain
Falls on slippery, icy pavement can also cause ankle injuries. When you struggle to recover your balance after slipping on ice, you can easily roll and twist your ankle. This may end up being a muscle injury whereby the tendon has been strained. Otherwise, a certain type of fracture in the ankle bone can result if more impact has been felt. This type of fracture can be caused not only by a fall on iced-over sidewalks, but also due to winter sports injuries.
Hip Fracture
Slips and falls on icy roads and sidewalks can result in many different types of broken bones, fractures and injuries. But one of the more severe injuries occurs when a fall is so hard and sudden that it fractures the hip bone. This can be a very difficult injury to repair, and it can also cause chronic, long-term pain. This injury especially affects seniors who are predisposed to osteoporosis or previous hip injuries. This injury should certainly be treated as an emergency by a physician.
Age Groups and Demographics Most Affected
Certain incidents and their resulting injuries may affect certain age groups more than others. It’s important to apply appropriate safety measures, so everyone can stay safe during the winter.
Children

Children are susceptible to falls. They can easily fall and injure themselves if they can’t reach handrails or don’t have proper balance. If your child experiences a fall, it’s important to first assess their head for any injuries and then check for elsewhere, like wrists and elbows.
Children especially enjoy their time sledding and tobogganing, which can put them at risk for injury. Be sure to always supervise kids during winter activities and provide them with helmets to protect their heads.
Seniors
Like children, seniors are also at a higher risk of slipping and falling on icy pavement. Seniors can easily lose their footing and take a fall that can put them in severe danger. Seniors who have suffered in the past from hip injuries could further damage their hips or back. Seniors should be accompanied and helped down driveways and across parking lots to ensure they are stable and have the support to walk safely. Seniors with mobility issues may want to consider motorized scooters during the winter months for extra safety precautions.
Adults With Previous Medical Conditions
Adults with previous back, neck and shoulder injuries are also at risk to be severely injured in any of these winter incidents. A slip or a fall can trigger a past injury and can cause further damage. Additionally, adults with a predisposition to osteoporosis are also at higher risk for broken and fractured bones if involved in a collision or a fall.
Active Adults
Adults who remain active throughout the winter months are also at greater risk for injuries if proper safety precautions aren’t followed. Adults who ski and snowboard should be advised that, without the proper equipment, they can be at risk for head injuries as well as neck, shoulder, knee and ankle injuries.
People who run in the winter should be advised to use properly cleared and salted trails and sidewalks, so they don’t risk slipping and falling.
Winter Injury Prevention Tips
Though many of these winter accidents can be quite common, they are easy enough to prevent by following specific steps.

- Thoroughly and regularly salt driveways, sidewalks and stairs
- Walk carefully across parking lots and provide children and seniors with additional support
- Stretch before performing any physical exercise
- Stay hydrated while exercising and shoveling snow
- Ensure proper footing when shoveling snow or scraping ice off the car
- Wear a helmet and protective equipment during winter sports
- Always supervise children playing outdoors in the snow
- Before shoveling or scraping, make sure to properly stretch
Most businesses and shopping centers take precautions to salt their parking lots and sidewalks once winter hits. Even still, patches may be missed or ice may have formed since the last salting. When rushing into stores and shopping centers, slow down and take your time to carefully walk across the parking lot. Look for areas that have been clearly salted or do not appear wet. Hold onto children and seniors to help stabilize them as you walk across the parking lot or driveway and indoors.
For back injury prevention, it is advised to stretch lightly at first, then move into a deeper stretch. If you are going to be shoveling snow, then it’s important to stay well-hydrated and take frequent breaks so as not to exhaust your body and muscles.
When performing winter sports and activities, be sure to always have the proper protective equipment, like helmets, to prevent head and other serious injuries. If you have access to a gym or can use a treadmill at home, it will prevent any risk of slipping and falling while running outdoors during the winter.
If you choose to run outdoors, go with a buddy and be sure one of you carries a cell phone to call for help in the event of an injury. Familiarize yourself with your running route ahead of time to ensure it’s an area that has been salted and cleared of ice and snow.
Winter Driving Safety Tips
Winter weather can make driving more difficult, which means it can put yourself and others at risk of injury. In order to prevent motor vehicle collisions, follow these winter driving safety tips:
- Have proper winter-grade tires installed on your car
- Store an ice scraper in your car
- Keep windshield washer fluid full
- Have your vehicle inspected, especially breaks
- Have a winter safety kit in your trunk, including a high-visibility safety vest, gloves and jumper cables
- Keep a first aid kit in your car
- Never drive without a cellphone
- Limit the time spent driving in the dark
What To Do If You Suffer a Winter Injury
If you or a family member suffers a winter injury, it’s important to first assess the severity level. Sometimes muscle injuries can be treated with ibuprofen and by applying ice or a heating pad (whichever is more comfortable) or taking a warm bath. However, more severe injuries will need to be treated immediately by a professional. If you suspect broken or fractured bones or a head injury, report it to a physician right away, visit the emergency room or visit your orthopedic injury clinic.
Educate yourself and your family about the potential incidents and accidents that can occur during the winter, and you’ll be much more prepared to prevent them. If a serious injury occurs, be sure to contact OIP to schedule an appointment with a doctor who can treat you for your specific injuries. Follow these winter injury prevention tips, and you can enjoy a happy and safe winter season.
Tennis Elbow vs. Golf Elbow Explained
-Causes of Tennis Elbow
-Treatment of Tennis Elbow
-Tennis vs Golf Elbow
If you’re experiencing regular pain when engaging in activities involving your forearm muscles, tennis elbow may be to blame. However, many patients confuse tennis elbow and golfer’s elbow. Here we will discuss different aspects of tennis elbow that will help you figure out if you may have this painful disorder. We’ll also highlight some of the differences between tennis and golfer’s elbow.
Tennis elbow can be quite uncomfortable, but the vast majority of patients will regain full strength and range of motion with proper treatment.
What Is Tennis Elbow?
Tennis elbow, also known as lateral epicondylitis, is a common overuse injury resulting from repetitive motion involving the tendons in your elbow. These tendons, the extensor carpi radialis brevis and extensor digitorum communis of the forearm, extend and stabilize the wrist as they anchor your muscles to your bones. When the attachment site weakens, you start to experience pain and tenderness while engaged in everyday activities involving gripping, grasping or lifting.
The first documented reference to tennis elbow was published in 1883, noting that frequent tennis players presented with pain in and around the elbow area of their racquet arm. Subsequent studies observed that using inappropriately matched equipment for one’s body size and muscle strength, gripping the racket too hard, hitting the ball off center and using poor technique on ground strokes increased the likelihood of tennis elbow pain.
What Are the Signs of Tennis Elbow?
Tennis elbow usually develops gradually, starting off as mild discomfort and worsening as time passes. In most cases, there is no specific incident that can be linked to the start of the symptoms.
Many people suffering from tennis elbow experience recurring pain radiating from the elbow all the way down the forearm, with pain that increases when they attempt to extend or straighten the elbow. Other common signs of tennis elbow include:
- Difficulty grasping or lifting objects
- Weak grip strength
- Sharp twinges when engaged in activities using the elbow
- Pain during and after activities involving the wrist
- Numbness or tingling in the fingers
- A dull ache when resting
Tennis elbow most often affects your dominant arm, meaning that right-handed people are more likely to develop tennis elbow in their right elbow and left-handed people are more likely to develop tennis elbow in their left elbow. However, it is possible for people to develop the condition in both arms. It is estimated that up to 20 percent of patients have some degree of bilateral tennis elbow.
Tennis elbow is usually considered degenerative rather than acute. If left untreated, tennis elbow can progress to the point where you have difficulty with simple everyday activities such as turning a doorknob, shaking hands, brushing your teeth or holding a coffee cup.
What Causes Tennis Elbow Pain?
Tennis elbow is most common in people ages 30 to 50, although the condition can be seen in people of all ages. Depending upon their activity level, children and senior citizens can be diagnosed with tennis elbow as well. There is no gender-related component to tennis elbow, and men and women are equally likely to be diagnosed with the condition.
Overuse is the most common cause of tennis elbow pain. When you frequently engage in activities that place stress on the tendon attachments and the muscle-tendon unit, microscopic tears form in the tendon where it is attached to the bone. These tears lead to the inflammation and pain associated with tennis elbow. Typically, overuse is defined as a high activity level three or more times per week with activity lasting 30 minutes or more per session. A poor overall fitness level can exacerbate the problems caused by overuse of the forearm and elbow area.
Tennis elbow pain can sometimes be linked to specific injuries or traumas. If you suffer a direct blow to the elbow, this could result in the swelling of the tendon and subsequent degeneration. When seeking treatment for your condition, it is important to inform your doctor of any injury or trauma that could be linked to the development of tennis elbow.
Finally, as with many medical conditions, genetics play a role in the development of tennis elbow. Some people are born with tendons that are naturally less durable, which makes them prone to developing the condition at an earlier age or in conjunction with pain in the shoulders and feet.
How Do You Get Tennis Elbow Without Playing Tennis?
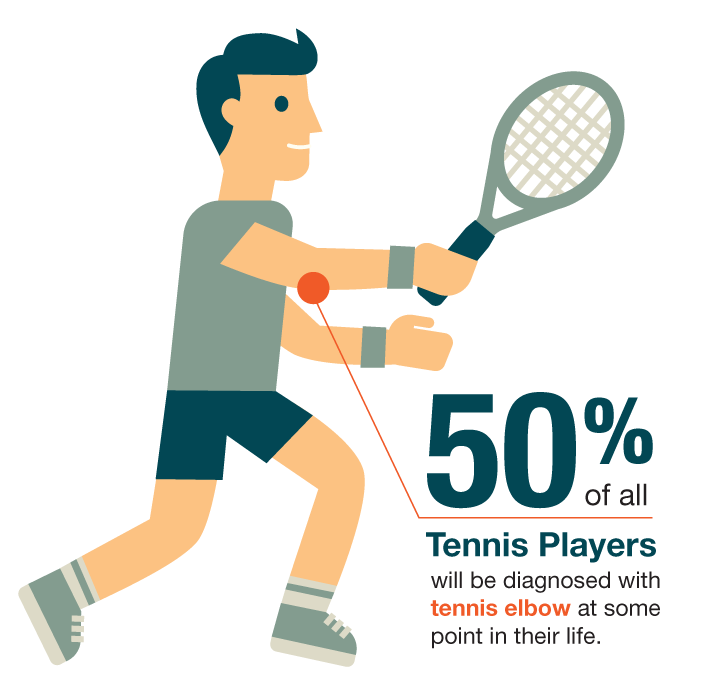
The Nirschl Orthopaedic Center reports that half of all tennis players will be diagnosed with tennis elbow at some point in their lives. However, people who play tennis make up less than 5 percent of all reported cases of the condition. This means the majority of people diagnosed with tennis elbow can attribute their condition to other causes.
Can you get tennis elbow from baseball and other sports, then? The answer is yes. Baseball pitchers are commonly affected by tennis elbow, especially if they haven’t been properly trained as to the correct pitching mechanics, frequently pitch curve balls or have a training schedule that is too vigorous. Younger players with elbows that are still developing are particularly prone to tennis elbow.
Other sports that have been linked to tennis elbow include football, javelin, discus, badminton and squash. The more frequently a person plays one of these sports, the more likely they are to develop the condition.
If you don’t play sports at all, you can still get tennis elbow from any sort of regular manual labor that involves lifting of the wrist and/or repetitive turning motions. This includes plumbing, meat cutting, painting and bricklaying, as well as typing. Hairdressers are also vulnerable to tennis elbow due to their frequent use of scissors, shears and other styling tools.
If you enjoy arts and crafts in your spare time, you may be vulnerable to tennis elbow due to the fine, repetitive hand and wrist movements involved in completing projects. For example, knitters and crocheters who work on projects for several hours at a time are prone to developing elbow pain. Scrapbooking can also be problematic due to the detailed cutting that is often involved.
How Is Tennis Elbow Diagnosed?
If you suspect that you may be suffering from tennis elbow, medical treatment is needed. Self-diagnosis can be dangerous, as tennis elbow is easily mistaken for other conditions. According to the American College of Sports Medicine, there are at least 43 different documented pathologies of the elbow joint. Many of these conditions, such as bursitis and arthritis, have symptoms that are similar to those of tennis elbow.
Tennis elbow is diagnosed based on a description of how your symptoms developed and what type of activities you engage in during a particular day. Your doctor will also consider factors such as whether you’ve previously injured your elbow and whether you have a history of nerve disease or rheumatoid arthritis.
During the initial examination, your doctor may ask you to perform basic tasks such as extending your arm fully straight and trying to straighten your wrists and fingers against resistance. If these tests are inconclusive, your doctor may order X-rays, an MRI scan or an EMG before making a final diagnosis. Bone scans may be done in rare cases to look for stress fractures or disease conditions that could be causing the elbow pain.
To assist your physician in obtaining an accurate diagnosis, it’s helpful to bring the following to your initial appointment:
- A written list of your symptoms
- Any questions you might have
- A list of any medications you are taking, including both prescription drugs and over-the-counter medicines
- A list of any previous surgeries you’ve had, as well as any injuries or other medical conditions that may be relevant to the pain you are experiencing
How Is Tennis Elbow Treated?
 Ice and anti-inflammatory, over-the-counter pain relievers such as aspirin or ibuprofen can provide temporary relief for your elbow pain. You will also want to rest the affected area as much as possible by stopping activities that irritate the tendon or by changing your technique to reduce stress on the forearm muscles.
Ice and anti-inflammatory, over-the-counter pain relievers such as aspirin or ibuprofen can provide temporary relief for your elbow pain. You will also want to rest the affected area as much as possible by stopping activities that irritate the tendon or by changing your technique to reduce stress on the forearm muscles.
Unfortunately, basic self-care at home will not resolve your tennis elbow pain permanently. The body requires new blood vessels and collagen proteins to heal the affected tendon.
Treatments for tennis elbow depend upon the severity of your pain, but may include:
- Cortisone Injections: Cortisone is used to control inflammation and relieve tennis elbow symptoms. They cannot be used long term, however. Too much cortisone can weaken sensitive tissues over time. Injections are given around the tendons and over the most painful point of the elbow, but are not directly injected into the tendon tissue itself.
- Bracing: When tennis elbow is linked to your occupation, it can be difficult to avoid activities that cause pain. In this case, functional bracing can be used to disperse forces that would normally be absorbed at the point of injury. Braces apply pressure on the muscles below the elbow to allow you to complete your daily activates with less discomfort. Tennis elbow braces are also called counterforce braces, and most commonly come in full elbow sleeve or simple strap styles that can be adjusted to provide the necessary tension around the forearm area. The braces can be worn throughout the day but should be removed before going to sleep at night.
- Physical Therapy: An experienced physical therapist can develop a personalized exercise program designed to strengthen the forearm, wrist and shoulder muscles while bringing in a new blood supply. The therapist may use massage, ultrasound and other muscle-stimulating techniques to promote healing. You might also be referred to an ergonomic specialist and/or occupational therapist if your condition is related to work activities.
- Surgery: According to the American Academy of Orthopaedic Surgeons, 80 to 85 percent of tennis elbow cases will improve after six months to one year of nonsurgical treatment. However, some patients may require surgery to remove the pain-producing tendon. After surgery, the arm is temporarily immobilized using a splint. The patient begins gradual strengthening exercises three to four weeks after the procedure, with the goal of being able to return to light athletic activity within four to six weeks and competitive athletic activity within four to six months.
Preventing Tennis Elbow Pain
Although tennis elbow treatment is very effective at relieving pain and improving range of motion, it’s possible for the condition to reoccur if the patient slips back into old habits. Modifying your daily routine is a key component of staying injury free.
If your tennis elbow is caused by work-related duties, it’s recommended that you speak to your supervisor or a company human resources representative about making accommodations to avoid a relapse. For example, if typing is the primary cause of your injury, you may need to type on a split keyboard to help your hands stay in a more natural line and use a wrist pad to keep your hands level with the keyboard at all times. You might also need to take more frequent breaks to allow for stretching and a change of positions.
If your pain is related to tennis or another sport, individualized coaching can help you refine your technique to prevent injury. In addition, a coach can check that your equipment properly fits your needs. For example, switching to a looser-strung tennis racquet reduces the stress on your forearm and keeps you from overworking your injured muscles and tendons.
Regardless of whether your tennis elbow is linked to work or recreational activities, you should make it a priority to follow through with the approved course of physical therapy. Strengthening your arm, shoulder and upper back muscles will help prevent future problems by taking stress off your elbow. Regular use of the exercises recommended by your therapist will allow you to maintain an active lifestyle without worrying about aggravating your injury.
TENNIS ELBOW VS. GOLFER’S ELBOW
You may have heard of both tennis elbow and golfer’s elbow before, but you probably don’t know what sets them apart. There’s a reason many patients confuse tennis elbow and golfer’s elbow. They share quite a few characteristics:
- Both are overuse injuries, caused by repetitive motions involving your arm and wrist.
- They both are characterized by damage to the tendons that attach your forearm muscles to the bone at your elbow.
- They both cause inflammation of the tendons but can progress to partial or full thickness tears of the tendon.
- Both cause pain to the elbow region.
- You don’t need to participate in the sport for which they’re named to get these conditions.
- Both start gradually but can get worse over time.
- Treatment for both is similar, beginning with giving your elbow and wrist a rest to reduce the amount of strain.
Despite these similarities, they are not the same conditions. In fact, they are quite distinct. Determining the correct cause for your elbow pain is the best method for receiving proper treatment. That’s why it’s important to visit your doctor who can assess your elbow and give you an accurate diagnosis.
WHAT IS GOLFER’S ELBOW?
Golfer’s elbow is a completely different disorder than tennis elbow. Medial epicondylitis, more commonly referred to as golfer’s elbow, is discomfort or irritation occurring on the inner side of the arm and elbow that is caused by activities that require repeated flexing or twisting of the wrist — for example, anything that requires you to bend your wrist downward or overuse your forearm muscles. When you do activities that require repeated lifting, especially if your elbow is extended and your palm is facing down, this can also cause the condition.
Despite the name, golfer’s elbow isn’t just limited to people who play golf. Repetitive tasks like gardening, shoveling, throwing a ball, painting and similar activities all put you at risk for golfer’s elbow. It can also be seen in weight trainers with poor technique, as well as those who work in an assembly line repeatedly bending and straightening the elbow. It is most common in people over age 40, smokers, those who are obese and those who perform repetitive activities for two or more hours per day.
People who are suffering from golfer’s elbow often experience pain when making a fist or twisting the forearm. In many cases, the affected area is tender to the touch or slightly swollen. If you are suffering from golfer’s elbow, pain often seems to worsen when you attempt to flex your wrist, pick up something with your palm down or squeeze a ball.
If the condition is not treated promptly, golfer’s elbow can cause weakness in the hands or wrist as well as stiffness in the elbow. The treatments for golfer’s elbow and tennis elbow are similar in most cases. One option is using a brace, but the best elbow brace for golfers elbow can depend on your symptoms and preferences. You will still need to seek medical care to learn the best way to handle your condition.
DIFFERENCES BETWEEN GOLFER’S AND TENNIS ELBOW
There is widespread confusion about how golfer’s and tennis elbow differ. And although they’re often confused, there are a few distinct characteristics of each condition that will help you tell them apart:
- Inflammation Location: The difference between golfer’s and tennis elbow centers on where the elbow is inflamed. A person suffering from tennis elbow will experience inflammation of the outside of the elbow and forearm areas, while a person suffering from golfer’s elbow will experience inflammation on the inner side of the arm and elbow.
- Tendon Affected: Tennis elbow affects the lateral (outside) epicondyle tendon. These are connected to the muscles that stretch your wrist backward and allow you to spread your fingers. Golfer’s elbow affects the medial (inside) epicondyle tendon. This is attached to the muscles you use to flex your wrist and contract your fingers, like when you grip something. This could present itself through inner elbow pain when you’re gripping or lifting something with your hand.
- Symptoms: The side effects of these conditions can be very similar, but they are on opposite sides of the elbow and arm. Tennis elbow presents with pain and tenderness experienced on the outside of your elbow, while golfer’s elbow can be felt on the inside of your elbow and down your arm. Golfer’s elbow can also cause numbness or tingling in your fingers.
GET HELP FOR YOUR TENNIS ELBOW PAIN
The goal of tennis elbow treatment is to help the patient regain total arm strength and endurance. Seeking medical care as soon as possible is the best way to get back to your daily routine. The medical experts at OIP will be able to diagnose your condition accurately, so you know definitively whether you have tennis elbow or golfer’s elbow.
Schedule an orthopedic appointment at OIP by using our online form or by calling 717-761-5530.
All About Seasonal Allergies & Joint Pain
In this article:
-Managing seasonal allergies
-How to prevent joint pain during allergy season
-Food Allergies and joint pain
Do seasonal allergies wreak havoc on your body?
If so, you’re not alone — many people experience an increase in their allergy symptoms during allergy season, especially when pollen counts are high. For some, symptoms are mild, with sneezing and stuffiness, while others experience joint, back and neck pain, in addition to breathing difficulties. However, although allergies can cause neck pain, join pain and back pain, there are many things you can try to make the pain subside.
In some cases, your symptoms may appear to be related more to the weather, injury or illness rather than specific allergens. However some allergy symptoms, such as non-allergic rhinitis and even joint pain, can be brought on by rapid changes in temperature and humidity that typically accompany the spring season. In the United States, spring often is the highest time for allergies, meaning your seasonal allergies could be the cause of your pain.
Let’s take a closer look at how allergies and joint pain may be related.
What Causes Back Pain?
Back pain is a common complaint, especially among adults. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, there are several potential causes of back pain.
Aging is one of the most common risk factors, as people may begin to experience back pain between the ages of 30 and 40. It is also a more prevalent issue among those who are not physically fit. Another risk factor is being overweight, which stresses the back and leads to pain. There are also hereditary factors, such as ankylosing spondylitis, a form of arthritis that can impact the spine. Back pain may also be caused by diseases such as cancer and arthritis.
Pain in the lower back is particularly common and is one of the leading reasons for people to go to the doctor or to stay home from work. Back pain can occur in acute or chronic forms. Acute pain is pain that begins suddenly and that typically lasts for six weeks or less. Chronic pain is more prolonged, such as pain lasting longer than three months. Chronic pain is less common than acute pain. It is possible for acute back pain to improve without treatment, depending on the underlying cause. You may find that taking ibuprofen, acetaminophen or aspirin can help to reduce your back pain.
There are several potential causes of back pain, including specific problems related to certain conditions or diseases:
- Arthritis
- Spinal stenosis
- Infections
- Kidney stones
- Scoliosis
- Muscle spasms
- Disk breakdown
- Ruptured disks
- Tense muscles
- Seasonal allergies
You may have more than one underlying cause linked to your back pain. If you have strong symptoms and aren’t feeling well, you’ll want to consider treatment options with your healthcare provider.
How Can You Treat Back Pain?
If you’re suffering from back pain, there are several potential treatments to consider.
Medications, like topical analgesic creams and ointments, may offer pain relief. Analgesic medications are over-the-counter medications, such as aspirin or acetaminophen. Nonsteroidal anti-inflammatory medications can reduce pain and swelling. These drugs often referred to as NSAIDs, include common over-the-counter medications such as ibuprofen and naproxen sodium. It is possible to get a stronger NSAID from a doctor.
If you have chronic back pain, additional medications may include muscle relaxants and even antidepressants. However, these options may not work for everyone.
Medications are just one treatment option. You may prefer to use hot or cold packs, or both, to ease a sore and stiff back. These packs offer a number of benefits. Heat helps reduce pain and muscle spasms, while cold reduces swelling and numbs more intense pain.
Exercise is another treatment option, especially if the cause of the problem is weight-related. However, it is important to note that while exercise can ease chronic pain, it is not ideal for acute back pain. Individuals suffering from either types of pain should seek advice and clarification from a doctor or physical therapist.
Joint Pain: You’re Not Alone

In a recent national survey, nearly one out of every three adults in the US reported having joint pain within the last 30 days. In this survey, deep pain was the most common complaint, followed by shoulder and hip pain
Joints connect your bones together, providing your body with support as you move. Joint pain can impact just about any part of your body, including the ankles, feet and hands. While joint pain can occur at any age, it becomes increasingly common as a person ages.
Damage to your joints caused by injury or disease cannot only interfere with movement, but can also be a common cause of pain. Some of the most common conditions leading to painful joints include rheumatoid arthritis, bursitis, osteoarthritis, gout, strains, sprains and other injuries, such as in sports.
As with back pain, joint pain can vary greatly in terms of severity in the amount of time that it lasts. For example, joint pain that resolves within a few weeks is referred to as acute. However, many people suffer from chronic joint pain, or pain that lingers for weeks or months at a time.
Other common causes of joint pain include:
- Osteoarthritis
- Tendinitis
- Overuse injuries, such as strains are sprains
- Gout
- Certain injuries, such as a fracture
- Infections caused by a virus
- Bursitis
- Autoimmune diseases, including lupus and rheumatoid arthritis
- Seasonal allergies
Can Joint Pain Be Treated?
To help understand joint pain, your doctor will first try to determine an underlying cause. Once you discuss the potential causes with your doctor, treatment options can vary based on the reason for the joint pain.
As with back pain, over-the-counter anti-inflammatory medication such as aspirin or ibuprofen may help with moderate to severe joint pain. If you have milder pain that is not accompanied by inflammation, it is possible that taking Tylenol for a short period of time will provide relief.
Other drugs that may help reduce joint pain include antidepressants, antiepileptic drugs and muscle relaxants that can treat muscle spasms. Some people may find relief by taking two drugs at once, such as muscle relaxants and NSAIDs. It is important to consult with a doctor before doing this.
Seasonal Allergies: Occurrence and Symptoms
Seasonal allergies are sometimes referred to as hay fever or allergic rhinitis.
In the United States, allergies typically are at their worst during the spring season, when flowers start to bud and trees begin to bloom. In most parts of the country, allergies typically start in February and can last until early in the summer.
Certain factors can influence the intensity and duration of allergy season. For example, milder winter temperatures can lead to early plant pollination. Additionally, a rainy spring can lead to rapid plant growth, ultimately causing an increase in mold and symptoms that can linger into the fall.
Seasonal allergies develop because the body’s immune system has become sensitized and is overreacting to something in the environment that normally does not cause problems in other people. Some of the most common triggers of seasonal allergies include grass, pollen and mold.
Some of the most common general allergy symptoms include:
- Nasal congestion
- Coughing
- Sneezing
- Wheezing
- Runny nose
- Itchy throat
- Itchy skin
- Itchy and watery eyes
- Hives
- Fatigue
- Joint, back and neck pain
Other factors can influence the severity of allergy symptoms. After a rainfall, pollen counts typically increase. Pollen counts are often higher on warm and windy days. On days with no wind, allergens are typically grounded. High humidity also promotes mold growth. In addition, pollen levels are generally at their highest in morning hours. Certain pollens, such as grass and ragweed, are most prevalent when the nights are cool and the days are warm.
Managing Your Seasonal Allergies

One of the most important things someone suffering from allergies can do is to identify the triggers. While some people seem to blame one trigger, it is possible that there are actually multiple triggers. It is not uncommon for those who suffer from spring allergies to show symptoms throughout the year. Some ways to avoid triggers include:
- Shower after being outdoors.
- Monitor pollen and mold counts, which are available on TV or in the news.
- Stay inside during peak pollen counts, which is the middle of the day of the afternoon.
- Wear a filter mask when working outdoors.
- Take preventive medication.
You can take other precautions as well, such as bathing and shampooing your hair each day to completely remove the pollen from your hair and skin. You should also wash your bedding in hot soapy water at least once a week.
You may need to wear sunglasses outdoors to protect your eyes from pollen. Those with severe allergies might find that a facemask is helpful during times when daily pollen counts are very high. It is also important to avoid line drying your bedding or clothes outdoors if the local pollen counts are high, as pollen can settle on these items.
Treatment options may include one or more medications to help control symptoms. While some drugs are available over-the-counter, others may require a prescription. Common medications to treat allergies include nose sprays and anti-histamines. Many people find that allergy shots provide relief, especially if their symptoms are linked to pollen. Allergy shots work by exposing the body to small amounts of allergens, which gives the body time to learn how to tolerate the allergens.
Can Seasonal Allergies Cause Body Aches, Back Aches and Joint Pain?
If you’re wondering whether seasonal allergies can cause back aches and joint pain, you’re not alone. There are plenty of ways seasonal allergies are related to back pain and joint pain as well.
For starters, it is possible to experience joint pain with a cold. Because both allergies and a cold cause similar symptoms, such as a runny nose and sneezing, itchy eyes and throat, and stuffy nose, some people confuse a cold with allergies.
Colds are typically accompanied by a sore throat and coughing, and maybe even a fever and body aches in your neck. However, some people who suffer from inflammation because of their allergies experience joint pain as the body attempts to flush out the allergen.
Can seasonal allergies cause joint inflammation?
Another potential link is that allergies can lead to fatigue, which can also make sore joints feel worse. Changes in weather can also lead to joint pain. This is especially true for cold and damp climates and weather-related changes that coincide with seasonal allergies.
Muscle and joint pain can be a coexisting problem resulting from arthritis, Lyme disease and certain immune disorders. It can also be linked to bursitis and osteoporosis. There are other potential causes as well.
If you experience sneezing and coughing as a result of your allergies, you may suffer from muscle, joint and neck pain due to the repeated sneezing or coughing. Seasonal allergies can also make you feel tired, which can ultimately make your symptoms worse.
If you’re not sure whether your joint pain is caused by allergies, the best way to distinguish symptoms is to take a short course of antihistamines. You can take antihistamines for a week to determine whether allergies may be a source for your pain.
How to Prevent Joint Pain During Allergy Season
There are many possible treatment options for allergies, which can keep joint and back pain at bay.
For airborne allergens, you might find relief through humidifiers, air purifiers, filters and conditioners. In addition, many people find that over-the-counter medications, prescription medications or a combination of both also offer relief.
Antihistamines are medications that help counterbalance the effects of histamine, the common substance in allergens that leads to allergy symptoms. Immunotherapy through allergy shots and anti-inflammatory nasal steroid sprays are another treatment option. These sprays work by reducing swelling and inflammation, which cuts down on mucus production. Nasal steroids work especially well when combined with antihistamines.
Decongestants, available in capsule form, help to reduce sinus swelling and discomfort by thinning nasal secretions. These medications are intended for short-term use and are often combined with antihistamines for full relief from symptoms.
Seasonal Allergies and Joint Inflammation
If joint pain occurs during allergy season, you can experiment with a variety of treatment options to find what works best for your joint pain. Over-the-counter medications such as Tylenol and Advil can work for mild pain. For acute pain, hot or cold packs might provide relief. Your doctor might recommend steroid shots, where medication directly into the joint to help reduce pain and inflammation.
Some individuals also find that physical therapy can help to strengthen muscles around the joint, which in turn strengthens the joint and improves the range of motion.
Food Allergies and Joint Pain & Inflammation
Seasonal allergies aren’t the only type of allergies that can contribute to joint pain. There are also certain pre-existing conditions and food allergies that can cause joint inflammation and your body to have inflammatory responses. Inflammation is what causes the joints to swell and create pain or discomfort. There are two main culprits for food-related joint pain:
- Arthritis
- Food allergy or sensitivity
If you already have arthritis, then you probably have experienced some amount of joint pain in the past. Although there are many different types, arthritis is basically inflammation that affects your joints, causing pain and stiffness. Some patients with this condition experience increased inflammation after eating certain foods. This is especially true of patients with rheumatoid arthritis, an autoimmune disease that causes chronic joint inflammation, especially in the hands and feet.
Even though arthritis causes your body to be in a constant inflammatory state, it’s important to be aware of the triggers that can cause bouts of increased inflammation and lead to painful joint symptoms. Some foods known to impact arthritic patients and cause joint pain include:
- Sugar: Releases inflammatory messengers called cytokines.
- Saturated Fats: This triggers fat tissue inflammation. Foods to watch out for are pizza, cheese, red meat, pasta dishes and grain-based desserts.
- Trans Fat: This is commonly found in fast food and processed foods like snacks, cookies, crackers, doughnuts and even margarine. Trans fat can trigger systemic inflammation.
- Omega 6 Fatty Acids: Although omega 6 fatty acids are essential to a healthy diet, arthritic patients should watch how much they ingest as it can produce pro-inflammatory chemicals. Omega 6 is found in mayonnaise, salad dressing and a variety of oils like corn, peanut, grapeseed, soy, sunflower and more.
- Refined Carbs: Products with white flour, white rice and white potatoes can fuel the production of advanced glycation end, which increases inflammation.
- MSG: Often found in prepared Asian food and other types of prepared foods, this chemical is a known trigger for chronic inflammation.
- Alcohol: Although alcohol most notably impacts liver health, it can also cause inflammation when not used in moderation.
If you don’t have arthritis, you may find that you experience pain in your joints after you eat certain meals. Foods can still cause joint pain if you have a food allergy or a sensitivity to particular ingredients. When you experience joint pain with no specific cause, then it may be time to take a closer look at your diet. There are a number of different tests a specialist can use to determine your own personal food and drink intolerances, such as:
- Food allergy/sensitivity test
- Stool analysis
- Elimination diet
- Nutritional deficiency test
Whether it be gluten, dairy or an assortment of other foods, identifying and eliminating these triggers from your diet could help you manage joint pain. An anti-inflammatory menu will also be beneficial to your overall health and well-being.
What if Your Pain Continues?
Despite your best efforts, you may find that your chronic pain does not resolve over time. This is especially true if you have already tried a combination of pain relief methods and treatment for allergies.
Your pain might be more than allergies. To be sure, schedule an appointment at one of OIP’s designated care centers today. We’re here to help!
Training for Spring Sports After A Long Winter’s Nap
Winter weather and holidays cause many people to take a workout break and pack on a few pounds, but there’s nothing stopping you from getting back in the swing of things. Getting back into shape after winter or any long break means easing in to your workout to prevent injury, and you can be ready for spring sports by planning ahead with a good training regimen and smart prep.
Get Your Space Ready
Despite that New Year’s resolution to lose weight and get back into shape, many people find themselves with a gym membership they’ve stopped using long before spring arrived. The first step in deciding how to get back into shape is finding a gym or space you’ll use.
To get the most out of your workout space, make sure it’s:
- Convenient to your work, home or school
- Open during hours you regularly have a break
- A space you pass almost every day
If you’re able to have a convenient, open gym that you see on a regular basis, it will stay at the forefront of your mind and be a little harder for you to skip, especially on leg day.
Start Slow: Spring Sports Preparation
Whether you kept busy during the winter or heeded Mother Nature’s call and tried your hand at hibernating, it’s best to begin slowly. Take stock of your current fitness level before you start working out so you avoid pushing too hard and causing an injury.
One way to assess your fitness level is by performing a variety of quick tests. They’ll give you a good idea of your aerobic and muscular fitness as well as help you better understand what areas you need to work on and take extra care with during your workout.
The activities you can do for your fitness assessment include:
- Measuring your body mass index (BMI)
- Measuring your waist circumference – around your bare abdomen, just above your hipbone
- Timing how long it takes you to walk one mile
- Recording your pulse before and after you walk that one mile
- Seeing how many pushups you can do at a time
- Sitting on the floor with your legs in front of you and seeing how far you can reach
These and other activities, such as monitoring how many sit-ups you can do, will help you determine where you are on the path to getting ready for spring sports. They’ll also point out where you need the most improvement.
Keep your training for spring sports to your own pace and don’t push yourself too hard too soon. For example, set a treadmill to the rate it took you to walk one mile when you begin your workout program and work up from that number. Don’t expect to double that rate in one day – that will likely lead to an injury such as a sprained ankle or damage to your knee’s anterior cruciate ligament (ACL).
How to Get Back Into Shape Every Day

A good schedule that allows for gradual improvement is the best way to get back into shape and avoid injury. To capitalize on this, try including some exercise into your routine each day. There are a couple of ways to do this:
- Schedule it. In an overly-scheduled world, it might be time to actually add a calendar appointment so you get reminders on your phone or email. This gives you a chance to block out the time for your workout and avoid double-booking. You won’t have to make the tough choice between appointments, and you’ll get the workouts in so you’re ready for anything from a competitive soccer league to company softball and kickball games.
- Build on what you already do. If schedules don’t provide you with a structured day, consider building in a workout to the activities you already do. This can mean taking your favorite book to the treadmill, doing sit-ups during the commercials of your favorite show, riding a bicycle to nearby appointments, or even parking at the far end of a parking lot every time you run an errand.
Thankfully, getting ready for spring sports is something many people are able to incorporate into their everyday lives.
Exercises for Spring Sports
The main thing to consider when starting back up after an exercise hiatus is to do less, even if you were able to do much more before. Reduce the amount of reps you do per set and reduce the weight you’re using. This makes it a safer workout, and you’ll be able to gradually work up to the level you may have been at previously.
There are, however, two important things to increase when first starting back: the warm-up and cool-down. Longer warm-ups will provide more blood flow to muscles and joints, reducing the risk of injury as you first get started. Lengthening the cool-down with a gentle aerobic exercise and lots of stretching will ensure you’re not causing any harm to those freshly worked muscles.
Stretches were hopefully a major part of your last exercise routine. This shouldn’t change. The more you incorporate gentle stretching, the safer you are. This is true whether you’ve been working out for one day or one decade. Stretching helps to prevent muscle and joint pain and damage, so always stretch it out.
If you’re looking for specific exercises that can help, we’ve created this list below. Please note that it’s always safest to have a professional show you how to do each exercise. Descriptions in articles and pictures on the side of a machine are rarely ever as good as having a live demonstration where someone can help you get the right motion and stop before any over-extensions.
Some exercises to get you back in shape include:
- Crunches
- Dips
- Leg Swings
- Lunges
- Hip thrusts
- Planks
- Pull-ups
- Push-ups
- Standing squats
- Step-ups
- Stretching before and after every workout
These exercises are great for strengthening muscles while you’re also getting in aerobic exercises such as jogging, swimming, biking, or even walking at a brisk pace. Your best bet is to find a professional to help you determine a workout that’s right for you and your current fitness level. Going too soft won’t give you the fitness you’re seeking, and pushing too hard often leads to injury.
Beyond working with a professional to set your schedule, there are also some other habits and spring fitness tips to consider when getting back into shape after winter.
Spring Fitness Tips: Mix It Up

One of the best spring exercise tips you can listen to is to make cross-training a major part of your routine. It’s hard to think about spring fitness without Spring Training coming to mind, and lots of the work there involves cross-training approaches.
Cross-training creates both individual training sessions and overall regimens that combine several different types of workouts. This gives a total body workout and allows you to focus on general health instead of muscle isolation. You’ll also get a combination of aerobic and anaerobic exercises that will help you build both muscle and stamina, which is required in most spring sports.
There are three major benefits to a cross-training approach, and these habits can help you get ready for any sport, just like the pros:
- Injury prevention. One of the most common reasons behind injury when training for sports is when someone focuses too much on a single activity. This laser-like focus puts a lot of pressure on muscles, joints, ligaments and other tissue without giving them a chance to repair and recover. Cross-training helps address this by building in rest days for certain parts of your body and using activities that address different muscle groups. Your body has time to rest where it’s needed, leading to a healthier training session and a healthier you.
- Conditioning. Most spring sports involve a lot of running and a heavy workload. To match the rigors of your sport, it’s best to put those requirements in your workout. Cross-training allows you to build this conditioning by switching up what you’re doing – that means less long-term rest and more demanding workouts than a standard arm day or leg day. Cross-training primes your body and allows you to focus on multiple goals in a single day. You can easily include activities that focus on building muscle mass, losing weight, and getting quicker on your feet.
- Active recovery. To prevent major injuries, you need to rest the muscle groups you’re focusing on. However, the active recovery schedule involved with cross-training allows you to still get a workout in while giving those muscles a break. It’s also a fun way to introduce new methods of training. Runners and football players use swimming to give their joints a break while building up strength with resistance exercises. Some studies even suggest that working out lightly or with different methods on a recovery day can improve your recovery time and help reduce the risk of injury because of increased blood flow and delivery of nutrients to sore or hurt muscles.
Give Yourself a Slow Down Time
Every workout day and week needs some time to breathe. Don’t focus so much on how to get back into shape that you forget about the overall concept of wellness. Too much of anything – even exercise – can be dangerous. Your body, your mind and your schedule will need some time to recover when you get back into the habit of working out.
Get ready for spring sports by planning your workout with large times between reps and activity switching. You don’t want so much time that your muscles cool down, but you do want to give yourself enough time to feel everything out as you go. The extra time will help you determine if a muscle has been injured or if a joint needs some relief. You’ll be better able to judge whether you’re finishing a set to feel the burn or pushing too hard.
You aren’t losing or giving up control; you’re just adding some time to be self-aware. This mindfulness is a top way to stay safe, and it’s a spring exercise tip that the majors all use.
Spring Fitness Tips: Listen to Your Gut
If your car engine needs oil, it doesn’t matter how much gas you put in the tank. The problem won’t be solved. Your body and your recovery work the same way, and nutrition is a major player in the world of getting ready for spring sports.
You’re training your body to last the whole season, so you need a strong foundation with the right mix of fruits, vegetables, meats and other healthy choices. Balance them right for your sport, and you’ll see a better workout recovery as well as a reduced chance your muscles will face injury.
Professional baseball players, for example, need to load up on a lot of protein to keep their muscles strong but also need a higher-than-normal amount of carbs and fats for energy. However, you probably won’t want to ramp up your diet to that extent until you get closer to professional-level status. But don’t worry if you slip up or are unsure of what you should eat; just follow the basic food pyramid to achieve an overall daily balance.
Even Michael Phelps, who was hitting a 12,000 calorie diet each day during the 2008 Olympics, is still fine-tuning his meals. He recently switched from a morning of grits, French toast, three fried egg sandwiches, omelets and chocolate chip pancakes to a slightly smaller menu of oatmeal, fruit, a ham and cheese omelet and some coffee. Those changes moved him toward more protein-dense foods and typically healthier items.
If you’re working out, eat. Limiting calories to also lose weight can increase the risk of injury and reduce the amount of energy you have to work out. Lowering your calories below a standard diet while working out may also slow your metabolism.
Give Yourself a Trophy

A loud, aggressive trainer is a great motivator for many people while they’re at the gym. If you need a little more motivation outside of the gym, treat yourself. Whether it’s simply acknowledging you’ve met workout goals and giving yourself a gold star or updating your clothes to help you feel fitter and happier, go for it.
One top benefit of spring sports preparation is that you’re getting better overall. Pick up some new cleats; grab a fresh bat, or get that pair of wireless headphones you spotted someone else wearing during a workout. These little trophies establish another layer of positive feelings toward working out, and they’ll help you keep the schedule.
You are your body’s boss, and everyone likes it when their boss shows a little appreciation.
What If You Push Too Hard?
Everyone in the gym has tried to break a personal record or get over that wall and ended up running right into it. With this, there often comes an injury that may involve a long recovery period if it’s left untreated. The most important spring exercise tip anyone can offer is: get yourself checked out whenever you have an accident and are hurt.
Not treating an injury can bench you for much longer than just the spring season.
For 24/7 orthopedic care assistance call 855-OUCH-OIP (855-682-4647) and then follow up your treatment with therapy and other activities suggested by one of our orthopedic providers. OIP offers a variety of treatment options throughout Central Pennsylvania that can help you get back on your feet after an accident.
From small procedures to help with pain management and physical rehabilitation, OIP can help provide you the best treatment for a spring training accident. OIP is here to help you with getting back into shape after winter, spring or any season.
Orthopedic Injury Clinic Closed for Easter Sunday
In observance of Easter Sunday, The Orthopedic Institute of Pennsylvania and Orthopedic Injury Clinic will be closed on Sunday, April 5, 2015.
Our offices will resume their regular schedules on Monday, April 6, 2015 at 8:00 am.
The Physicians and Staff would like to wish you and your family a happy Easter!
Orthopedic Injury Care Hotline
For acute orthopedic injury advice and care, call: 855-OUCH-OIP (855-682-4647).