Dr. Nathan Angerett to Give Talk on Arthritis of the Knee & Hip
Date: Wednesday, August 9th 2023
Location: 125 State Road Mechanicsburg, PA 17050
Time: 6:00 pm EST
RSVP to Wendy Crecelius at wcrecelius@oip.com or 717-980-3593.
Guide to Hip Pain Relief and Treatment Options
Hip pain and discomfort might be caused by a minor strain or could be due to a chronic condition. Whatever the cause, hip pain can impact your quality of life and keep you from doing the activities you love. To effectively treat your hip pain, you’ll want to know its causes. From there, you can work out how to address the pain and decide if it’s necessary to see a doctor.
This guide to causes and hip pain solutions can help you determine how to get the relief you need.
Causes and Symptoms of Hip Pain
Hip pain can result from the following conditions and causes:
Arthritis
Different kinds of arthritis can cause hip pain. For example, osteoarthritis, common in older adults, is the result of wear and tear. Inflammatory arthritis can affect people of any age and cause a wide range of symptoms, including hip pain.
The symptoms of arthritis affecting the hips can vary. Some people experience a dull aching pain that spreads to other areas of the body, such as the groin, buttocks or thighs. Other people may experience severe pain that limits their range of motion and makes it difficult to walk.
Bursitis
Bursae are small fluid-filled sacs located in various areas of the body, including the hip. Their job is to reduce friction, but sometimes these sacs become inflamed in the case of a condition called bursitis. Bursitis typically causes pain in the hip, but over time it can cause a dull, aching pain to spread to the thigh.
Tendonitis
Tendons are tough fibers that connect muscles to bones throughout your body. When these tendons become inflamed, the condition is referred to as tendonitis. Tendonitis in the hip can cause swelling, affect movement and create a grating sensation when you walk.
Hip Dysplasia
Hip dysplasia is a condition in which the bones of the hip joint are misaligned, leading to the joints wearing out faster than they would if properly aligned. The condition can affect children, adolescents and adults. As the joint wears out, you can experience stiffness and pain.
Injury
Injuries to the hip can also result in pain. A fracture, dislocation or labral tear are among the potential injuries to the hip point. A fracture might be the result of a fall and is common among older people. Hip dislocation occurs when the femur slips out of the hip socket, which may happen as the result of a fall or a car accident. The labrum is a ring of cartilage that helps to cushion the hip joint. A labral tear is a common sports injury.

Pain Treatments and Remedies for Hip Pain
Some conditions causing hip pain can be treated and resolved at home, while others require medical intervention. Some of the common remedies for hip joint pain include:
- Over-the-counter medication: Minor hip injuries, such as a strain, can benefit from over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin.
- Ice and heat: You may also find relief from hip pain by using ice and heat. Apply an ice pack to the affected area for short intervals. You can also soak in a hot bath or use a heating pad to ease the discomfort.
- Stretching and low-impact exercises: Stretching and low-impact exercise, such as yoga, can help strengthen hip muscles, reduce pain and prevent future pain. Exercise as an approach to pain relief is ideal for minor discomfort and injury. If you are experiencing severe pain or you aren’t sure of the cause of your hip pain, it is best to consult a doctor before trying stretches and exercise at home.
- Physical therapy: A doctor may decide that you could benefit from physical therapy. A trained physical therapist will show you how to engage in stretches and exercises to address and reduce your pain.
- Cortisone injections: Some conditions require more intervention. Your doctor may suggest cortisone injections to reduce pain and swelling in the hip joint. Injections can be a treatment option for conditions like bursitis and osteoarthritis.
- Surgery: Some hip conditions require surgical intervention. For example, a labral tear may need to be repaired via minimally invasive surgery. Osteotomy is another example of hip surgery, usually done to treat hip dysplasia.
When You Should See a Doctor
Hip pain might be a minor inconvenience that resolves over time, or it could be the result of a more serious condition that requires treatment. It might be time to see a doctor if you experience:
- Intense, sudden pain after an injury: Injuries sometimes happen while you are playing a sport or after you have fallen, and it is always a good idea to be checked by a doctor if you experience sudden pain. A hip dislocation, fracture or labral tear requires prompt medical attention. If it turns out to be a less serious injury, a doctor can still recommend appropriate care.
- Chronic pain: Some hip pain may feel like a dull ache that developed over time. If that pain stubbornly consists over weeks or months, it may require medical attention. A doctor will be able to discuss your symptoms and order appropriate diagnostic tests to find the cause of your chronic hip pain.
- Swelling: Some minor hip conditions, such as tendonitis, may cause swelling, but swelling can also be a sign of something more serious. If you notice swelling or discoloration at the site of pain, it is a good idea to have the injury evaluated by a doctor.
- Signs of infection: Pain accompanied by warmth, redness and swelling could indicate an infection in the joint, which can have serious consequences if left untreated.
- Difficulty moving: If your pain impedes your ability to move the joint or walk, it is time to make a doctor’s appointment. Pain that interferes with your day-to-day life requires treatment.
Receive Care for Your Hip Pain at OIP
If it is time to seek treatment for severe hip pain, where do you start? Orthopedic Institute of Pennsylvania (OIP) has a Hip and Knee Medical Center that specializes in the care of those two vital joints. Our providers offer conservative treatment for hip pain, including medication, physical therapy and injections. If you do need surgery to address the source of your pain, our team is here to offer rehabilitation services to get you back on your feet.
Contact us today so we can determine the best way to get you the hip pain relief you need.
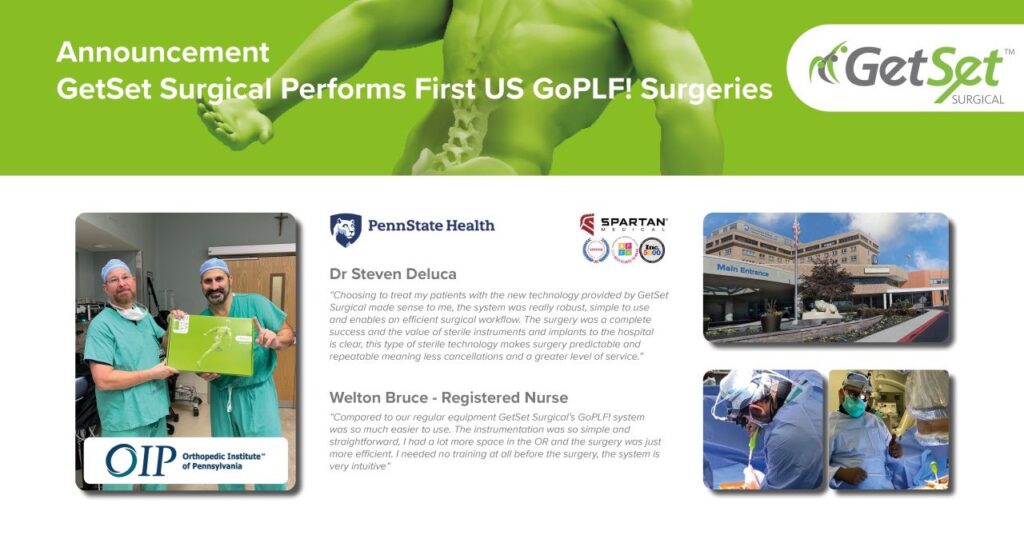
Dr. Steve DeLuca and Dr. John Kelleher Performs the First 2 GoPLF Surgeries at Penn State Health
Causes of Ankle Popping and Clicking
No matter your age, you might have heard a crackle or pop in your joints when sitting down, standing up or simply walking. Luckily most popping cases are not detrimental to your physical health. However, if left untreated, they could cause mobility complications.
Medically, popping in your joints is known as crepitus. If you’re experiencing a bout of crepitus, it could be from overworking your joints through exercise or stiffness in the joints after a long period of inactivity. While these causes may sound contradictory, it’s how our bodies adapt to certain stimuli — or lack thereof.
At the Orthopedic Institute of Pennsylvania, we can treat foot and ankle pain. Learn more about our services below.
Why Does My Ankle Keep Popping?
Ankle popping on its own is very common. If your popping ankle isn’t painful, it is likely caused by a gas release or tendon rubbing. However, if it is accompanied by pain or swelling, there may be an underlying cause.
The most common causes of ankle clicking or popping include:
- Gas release: Every time your ankle moves, the joint capsule filled with lubrication fluid is stretched. The fluid in the capsule can contain bubbles of nitrogen that can pop when you move, causing a loud popping sound — similar to when you pop your knuckles in your hand. Tight muscles can also contribute to gas buildup in the fluid, especially after inactivity like sleeping or binging a TV show. This is normal and does not signify an underlying cause.
- Tendon slip: The peroneal tendons in the lower outside of your leg work to stabilize the ankle joint. Sometimes, these tendons slip from the muscle surrounding them, resulting in a snapping sound or feeling. A recent ankle injury could increase the ankle popping frequency. This is also common and not a cause of concern unless it is painful.
Less common reasons that may signify an underlying health condition include:
- Tendon dislocation: The peroneal muscles surrounding the tendons can be pushed from their usual location, causing popping and snapping sounds in your ankle every time you move. This can happen during an ankle sprain. The inflammation, swelling and pain that occurs will need medical attention.
- Osteochondritis dissecans: This condition causes a small segment of bone to separate and causes the cartilage in the ankle joint to wear away. This cracking sound could be painful after a lot of movement, like walking or running.
- Osteochondral lesion: Lesions can form on the cartilage on the ends of your joint bones. Clicking and locking the ankle can occur, limiting the range of motion and causing swelling.
- Ankle osteoarthritis: Osteoarthritis refers to a joint deterioration similar to osteochondritis with the wearing down of joint cartilage over time. While most common in the knees, it can also occur in the ankle.
- Peroneal tendon injury: The peroneal tendons that may slip to make a cracking noise can also become injured.
Prevention and Remedies of Ankle Popping and Cracking
You can do several exercises at home to strengthen your popping ankles. These stretches both prevent ankle popping and reduce cracking sounds that already exist.

Ankle Circles
Performing ankle circles can warm up your joints and increase mobility. You can do this exercise from a seated or lying position:
- Sit or lay with your legs stretched out front. Prop your leg on a stable surface with the ankle hanging off the edge.
- Rotate your foot in clockwise circles 10 times with your ankle.
- Switch to counterclockwise circles 10 more times.
- Swap feet and repeat with the other ankle.
Towel Stretches
Relieve tight ankles with these simple towel stretches you can do at home:
- Sit on a flat surface with your legs straight out in front of the body.
- Loop a towel horizontally around the sole.
- Gently pull the towel ends toward the body, stretching the foot.
- Hold this position for 20 seconds.
- Repeat as needed.
Calf Raises
Strengthen your calf muscles to reduce pressure on the ankles in motion.
- Stand on the edge of a platform or the bottom stair step with the heels hanging off.
- Slowly rise onto the toes, driving the body fully upward with the calves.
- Let the heels gently fall, stretching slightly below the ledge.
- Repeat 10 times.
When to See a Doctor
When your ankle popping begins to cause discomfort or pain, consider getting a proper diagnosis from a doctor. They may order tests like an MRI or CT scan to look inwardly at the bone and cartilage.
If you recently had an ankle injury, rest is a major proponent of healing. A doctor may recommend anti-inflammatory medications to help with the pain and swelling.
A doctor can stabilize the ankle with a brace or orthotic to promote faster healing for more serious conditions. Physical therapy also works alongside any stabilization devices to slowly get your ankle back to regular functioning. If necessary, surgical options are available, including arthroscopy and total joint replacements.
Visit the Orthopedic Institute of Pennsylvania Today
At the Orthopedic Institute of Pennsylvania, our ankle and foot care center is committed to helping you regain full mobility. For more information on how our services can benefit you, contact us today!
Tips on How to Prevent Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) happens when constant pressure is put on the median nerve. This nerve runs from the forearm through the wrist and provides feeling and sensation to the whole hand — palm, fingers and thumbs.
If you have carpal tunnel, you will notice numbness or tingling in your hand. You may also experience weakness in your affected hand, occasionally dropping items from a loose grip. CTS has no leading cause, as it results from anything that can squeeze or cut off circulation in this nerve.
How to Avoid Carpal Tunnel
Incorporate some of the following methods into your routine to help prevent the development of carpal tunnel. Be sure to talk to your doctor about other options or exercises you can try.
Relax Your Grip
Sometimes, we don’t notice how tightly we are tensing up our hands until it’s too late. While gripping something, become aware of the strength needed to hold it and don’t overexert. For example, if your work involves typing, hit the keys softly rather than punching them. If you prefer to handwrite, consider using a bigger pen with a soft adapter for easy grip.
Stretch Your Fingers
It is important to get up and stretch your legs every so often, and do the same for your hands! If you consistently use a computer mouse, ink pen or other office materials, there is likely pressure on your median nerve. Gently stretch and bend your wrists periodically to give them a bit of a hiatus.
Improve Your Posture
Sitting in a forward hunch harms your back alignment and nerves. Rolling your shoulders forward can shorten your neck and shoulder muscles, compressing the nerves in your forearms. Keep proper posture to maintain healthy nerve function.
Carpal Tunnel Treatments
If you already have carpal tunnel, you can get help from several available treatments. Nonsurgical approaches are usually the first choice, but surgical options are the next resort if the pain worsens.
Nonsurgical Treatment Options
The Orthopedic Institute of PA offers multiple nonsurgical options for our patients. Physical and occupational therapies are the standard choices. You will walk through a series of exercises and use splints to regain your hand and wrist’s full range of motion.
Additionally, we offer Xiaflex nonsurgical solutions, which are an injection to help improve hand and wrist function.
Surgical Treatment Options
Surgical approaches are best for severe carpal tunnel symptoms. We offer:
- Endoscopic carpal tunnel release
- Arthroscopic surgery
- Joint replacement
Recovery
Your hands are one of your most used body parts, so they must receive the proper healing time. Full recovery from carpal tunnel treatments can last from weeks to months, depending on the severity of the condition. If surgery is used, physical therapy is a standard follow-up to ensure the procedure went smoothly and the full range of motion is returning.
Schedule an Appointment with the Orthopedic Institute of Pennsylvania
Contact the Orthopedic Institute of Pennsylvania for more information, and set up an appointment for carpal tunnel treatment.
New OIP Carlisle Walk-In Clinic is Open!
Carlisle Walk-In Clinic
CARLISLE, PA (September 12, 2022) – The Orthopedic Institute of Pennsylvania (OIP) is pleased to announce the opening of its new Walk-In clinic in our Carlisle location, offering neighbors in and around the area with increased access to orthopedic emergency services such as strains, sprains, fracture or dislocation.
Our Walk-In Clinic hours are Monday through Friday, 8:00 am to 4:30 pm.
Skip the ER and come see us at 250 Alexander Spring Rd in Carlisle!

Reasons Why Physical Therapy Is So Important

Physical therapy benefits people of all ages who experience medical conditions, injuries or illnesses that limit their motion and daily function. Professionals customize a person’s physical therapy program to help them return to their prior level of functioning. They might also encourage lifestyle changes that prevent further injury and strengthen the patient’s overall health and well-being.
Learn why physical therapy is important, its various benefits and how physical therapists identify, diagnose and treat movement problems below.
Who Can Benefit From Physical Therapy?
Anyone can benefit from physical therapy — even those who have specific conditions but are currently pain-free. Physical therapists can identify and address potential problems that could lead to pain or injury in the future. They can provide supplementary treatment for various medical conditions, depending on their specialty.
For example, physical therapy can benefit those experiencing the following injuries or types of pain:
- Arthritis
- Back pain and strains
- Herniated disc
- Knee pain
- Rotator cuff tears
- Sciatica
Patients might go to physical therapists for specific sub-specialties, such as pediatrics, sports, geriatrics, cardiac, neurology or respiratory physical therapy. For instance, a pediatric physical therapist specializes in helping children with particular injuries or conditions like inherited movement disorders or bone and muscle issues. A cardiac physical therapist provides rehabilitative exercise counseling for those recovering from heart failure, a heart attack or heart surgery.
How Physical Therapists Identify, Diagnose and Treat Movement Problems
Your primary care doctor may refer you to physical therapy to help manage an issue. Physical therapists can then identify, diagnose and treat the pain to help you maintain or restore your range of motion:

- Discussing your symptoms: Physical therapists will first speak with you about your pain or injury. They might discuss your habits or events that may have led to your symptoms. The conversation can help them determine how you may have gotten where you are physically.
- Physical assessment: Next, you’ll undergo several functional tests to identify the source of your pain or injury. These tests measure your strength and range of motion, either throughout your entire body or the specific muscles and joints causing the problem.
- Diagnosis: Physical therapists then compare your conversation and physical assessment to determine the cause of your issues.
- Treatment plan: Finally, physical therapists explain your diagnosis and customize a treatment plan to help you manage the problem. From therapeutic exercises and manual therapy to newer techniques, a physical therapist will employ several noninvasive treatment options to address or prevent movement issues.
After your initial evaluation, treatment might include stretches or exercises to improve your strength and mobility while helping you stay pain-free. You’ll also be encouraged to continue rehabilitation with at-home exercises. Your physical therapists will assess your condition throughout your sessions to ensure your progress.
Physical Therapy Benefits
So why is physical therapy important? People use physical therapy for various reasons. It may be time to consider physical therapy when you have persistent joint achiness or muscle burning that can’t be relieved with at-home remedies.
Physical therapy can help:
- Reduce or eliminate pain: Physical therapists can help relieve pain caused by injuries or illnesses. Several exercises or manual therapy techniques like joint and tissue mobilization or ultrasound and taping methods can reduce pain, restore muscle and joint function and prevent the pain from returning.
- Avoid surgery: If physical therapy can help you eliminate pain or recover from an injury, you might not need surgery. Even when surgery is required, physical therapy can help you improve your strength beforehand so you can recover faster.
- Improve strength and mobility: No matter your age, if you have issues standing, walking or moving, physical therapy can help. Strengthening and stretching exercises can help restore your movement. You might also use assistive devices like canes or crutches in treatment. Since therapists customize your care plan, they can adapt any important activities in treatment to ensure your maximum performance and safety.
- Recover from a stroke: It’s common to lose some degree of movement and function after a stroke. Physical therapy can help you improve your gait and balance while strengthening the weakened parts of your body. Physical therapists can also improve stroke patients’ ability to move around the home so they can be more independent and require less assistance for activities of daily living.
- Recover from or prevent a sports injury: Physical therapists understand sports can increase your risk of specific injuries, like stress fractures for runners. They’ll design recovery or prevention exercise plans to ensure a safe return to your sport or to help prevent injuries while you’re playing.
- Improve your balance and prevent falls: When you begin physical therapy, therapists will evaluate your risk of falling. They’ll help improve coordination with exercises or assistive devices to promote safer walking. If a vestibular issue causes a balance problem, therapists can employ specific methods to restore vestibular functioning and reduce dizziness.
- Manage age-related issues: Individuals may develop specific bone or muscle conditions like arthritis or osteoporosis as they age. Physical therapists can help patients recover from joint replacement and help them manage their conditions.
How to Get Care for Your Physical Therapy Needs
Our priority at the Orthopedic Institute of Pennsylvania is providing high-quality care and service to address your physical therapy needs. Our friendly, highly skilled team works with you to achieve a higher success rate and improve your overall quality of life.
At our physical therapy center, you can expect specialized services and treatment in areas like:
- Orthopedics: Orthopedics address musculoskeletal injuries and impairments.
- Sports medicine: This specialty focuses on treating and preventing sports-related injuries.
- Hand therapy: Despite the name, hand therapy focuses on the hands, arms, wrists, elbows and shoulders.
- Work-related injuries: This treatment aims to help patients safely return to work.
We design our individualized treatment plans to fit your condition and lifestyle. We use expert hands-on manual techniques, such as joint and soft tissue mobilization. With these techniques, we can help you improve function, increase your range of motion and reduce pain, swelling and inflammation so you can get back to the activities you love the most.
Work With OIP as Your Physical Therapy Provider
You might need physical therapy for several reasons, from illness to injury. For your physical therapy needs, turn to OIP. By providing early intervention and 24-hour access to care, our customized treatment plans can help you restore your mobility as quickly as possible.
Our patients are our top priority. We provide high-quality care, work with all insurance providers and offer convenient scheduling to fit therapy around your busy schedule.
Use our online appointment request form to make an appointment today.
Ways to Alleviate Joint Pain
Jump to:
Joint pain can occur in various body parts, including the shoulders, knees, and hips. Previous joint injury, weight, age, underlying medical conditions and joint overuse can increase the risk of developing joint pain. While joint pain may be constant, it can also occur episodically.
Along with pain, you may notice your joints feel sore, achy or stiff, with a limited range of motion. Severe joint pain may cause throbbing, burning or grating sensations. Fortunately, numerous joint pain solutions minimize joint pain and inflammation and restore a proper range of motion.
Natural Remedies
Many natural or at-home remedies provide relief for joint pain. Generally, natural remedies are often the first line of treatment people consider when they experience joint pain, while more severe pain may require professional intervention. Many at-home treatments are effective for mild to moderate pain. Some of these at-home joint pain solutions include:
Ice and Heat
Ice and heat therapy is an effective joint pain remedy that can alleviate joint pain, discomfort and inflammation. Applying an ice pack to a sore joint can improve swelling and painful symptoms. Generally, experts recommend icing a painful joint for 15 minutes two to three times a day or as needed to improve symptoms. Physicians recommend applying ice first before heat therapy when joint pain becomes noticeable.
After a day or two, you can apply a heating pad or hot water bottle to improve joint pain and alleviate any muscle spasms. If you don’t have a heating pad, you can take a hot shower, bath or even immerse a painful joint in a basin of hot water. When using heating pads, you should only apply the pad directly to the joint for 20 minutes at a time.
Rest
Rest is essential for joint and muscle pain relief and can take the strain and pressure off an injured or damaged joint. If you notice pain in a joint, you should rest the joint immediately and avoid any activities that may aggravate joint pain. Rest can reduce inflammation and swelling around the joint and alleviate pressure.
While exercise can help a painful joint, knowing when rest is necessary is important. If exercise or simple movements are causing pain, discomfort or limited mobility, you should rest the joint for at least one day. Rest, along with ice and heat therapy, can minimize joint pain. After symptoms improve, you may continue gentle exercises to strengthen the joint and surrounding muscles.
Exercise
Exercise is another important solution for joint and muscle pain relief. It is important only to exercise if you are not experiencing severe joint pain or related symptoms. Exercise can improve flexibility, increase strength and minimize joint pain and stiffness.
Swimming is an excellent exercise for those with joint pain because aquatic activities alleviate pressure and strain on sore joints. While exercise may seem intimidating for those with joint pain, exercising can maintain bone strength, enhance balance, keep an ideal weight and provide energy for the day.
Medical Remedies
Many patients may need medical remedies for moderate to severe joint pain. If you don’t experience relief from at-home treatments, you may want to see your physician and learn more about common medical remedies for joint pain. Some of the most common medical treatments to improve joint pain include:
Corticosteroid Injections
Corticosteroid injections can ease joint pain and minimize inflammation around the joint, preserving the joint’s function. Corticosteroid shots use anti-inflammatory medication to improve various medical conditions, including joint pain and stiffness.
When corticosteroid shots are injected into the joint, the medicine helps minimize inflammation, alleviating pressure on the joint and surrounding structures. Corticosteroid injections can provide joint pain relief from six weeks to six months, depending on your symptoms.
Physical Therapy
Physical therapy is another beneficial treatment for joint pain that can stabilize a joint while strengthening the surrounding muscles. A physical therapist can help you regain a proper range of motion with gentle, guided exercises and stretches. Physical therapy is often combined with cold or heat therapy for the best results.
While physical therapy is quite effective for improving joint pain, it is most effective when combined with proper diet and other joint pain treatments. During physical therapy, you will learn low-impact exercises that improve joint pain and prevent further discomfort.
Over-the-Counter Pain Medicine
Over-the-counter (OTC) pain medication can minimize discomfort and improve pain-related symptoms for general joint pain and discomfort. Certain OTC medicine can reduce inflammation, improving swelling and joint pressure. Common OTC pain medicine includes aspirin and ibuprofen.
If you take other medications, you should consult your physician before adding any OTC pain relievers. If you don’t need an OTC pain reliever for swelling, you can use acetaminophen to reduce pain. When taking acetaminophen, you should avoid drinking any alcohol.
Types of Joint Pain
The joints are the connection between bones, providing your body with support as your move. When a joint becomes damaged or injured, it can cause pain, discomfort, swelling and limited mobility. Research suggests approximately one out of every four adults in the United States are affected by joint stiffness or pain.
While acute joint pain typically only lasts a few weeks, chronic joint pain can last for months and frequently occur in episodes. Even acute joint pain can negatively impact your overall quality of life. Understanding where your joint pain is located and what may be causing the discomfort can help you find an effective treatment. Some of the most common types of joint pain include:
Knee Pain
The knee is a common joint in the body that can become sore or painful. Knee joint pain can develop from an injury or age as the joint begins to wear down. Knee joint pain often causes an inability to fully extend or straighten the knee and difficulty placing full weight on the knee.
You may notice knee instability, weakness, stiffness or inflammation with knee joint pain. Other common symptoms of knee joint pain include redness, popping noises and the skin being warm to the touch. Approximately 25% of adults experience chronic knee pain.
Shoulder Pain
Approximately 18% to 26% of adults experience shoulder pain at any point in time, meaning it is one of the most common regional pain conditions. The shoulder is a complex joint designed to rotate 360 degrees. While the shoulder joint is impressive in its mobility, it may be prone to pain or stiffness.
Initially, shoulder pain may start as a mild, dull ache and slowly worsen over the next few days or weeks with continual use. Moderate or severe shoulder pain may develop suddenly with more noticeable symptoms. Shoulder joint pain may cause grinding sensations, limited movement and tender redness or inflammation.
Hip Pain
The hip joints are the body’s largest ball-and-socket joints, allowing for fluid movement. The hip joints connect the thighbones to the pelvis, allowing you to walk, run, stand and sit. While the hip joint can withstand repeated use, these joints can become painful and sensitive if they experience too much wear and tear.
Contact Orthopedic Institute of Pennsylvania
At the Orthopedic Institute of Pennsylvania, our providers are experts in all aspects of orthopedic care and are dedicated to providing the highest level of patient care. We are proud to offer innovative treatments for back pain, foot pain, hand pain and neck pain.
Request an appointment online today to learn more about joint pain and joint pain treatments.
Signs Your Foot Pain is Serious
-Types of Foot Pain
-Other Causes of Foot Pain
-Symptoms That Warrant Medical Attention
In many ways, your feet are your body’s unsung heroes. They support the weight of your body each day, and they take you where you want to go one step at a time.
So when you experience foot pain and other problems, it can keep you from doing the things you want to do. Here are some of the possible reasons your foot pain may be occurring, possible treatment options and when you should see a doctor.
Types of Foot Pain and Treatment Options
Foot pain can occur in different parts of the foot due to various conditions, and the location of your foot pain can inform you of the cause — anything from shoes that don’t fit correctly or trauma to the foot to chronic arthritis, diabetic neuropathy or prolonged strain on the tendons, also known as a repetitive strain injury (RSI).
The treatment options for foot pain also vary depending on foot pain cause and severity. We’ve organized some common foot pain causes and their treatment options below according to where they occur on your foot.
Heel Pain
One area of the foot that is prone to pain is the heel. Causes of heel pain include:
- Plantar fasciitis: Plantar fasciitis is an RSI that’s common among runners or people who are often on their feet. It occurs when the ligaments along the arch of your foot between your toes and heel become stretched and inflamed. To treat plantar fasciitis, your doctor will likely suggest orthotics, rest, non-steroidal anti-inflammatory drugs (NSAIDs) and physical therapy. If the pain is intense, they may offer corticosteroid injections. Surgery is rarely needed.
- Heel spurs: Heel spurs occur when excess bone tissue grows on the underside of your heel near your arch. The stress inflicted on the heel from plantar fasciitis is the most common cause. Treatment for heel spurs involves rest, custom-fitted shoes, corticosteroid injections or surgery.
- Heel fractures: Heel fractures are almost always serious injuries caused by trauma from a fall or another accident. Bruised and swollen heels that you have trouble walking on are common signs of a heel fracture. Treatment involves extended rest, splints or casts, physical therapy and surgery if the pain continues.
Other causes of heel pain could include a ruptured Achilles tendon, Achilles tendinitis, stone bruise or psoriatic arthritis.
Ball of the Foot
Common causes of pain in the ball of your foot include:
- Sesamoiditis: If the ball of your big toe causes you pain, you might have sesamoiditis. In that space are two small bones called sesamoids. When the tendons that connect those bones become inflamed from overuse, sesamoiditis occurs. To treat this RSI, your doctor will likely recommend rest, orthotics, NSAIDs, tape to immobilize the big toe and corticosteroids if you experience intense pain.
- Morton’s neuroma: High heels, small-fitting shoes, being on your feet for extended periods or all three together are common culprits of Morton’s neuroma. This condition occurs when non-cancerous tissue builds up between the metatarsal bones located beneath your ankle to the balls of your feet. This tissue pinches the nerves between those bones. Initial treatment for Morton’s neuroma involves rest and footwear changes. You may need corticosteroid injections or surgery in rare cases if symptoms persist.
- Metatarsalgia: Like Morton’s neuroma, shoes that are too small can cause metatarsalgia, or inflammation in the ball of your foot. Treatment involves over-the-counter (OTC) pain relievers, ice packs, comfortable footwear that fits and shoe inserts to relieve pressure.
Pain in the ball of your foot could also indicate a metatarsal fracture or sprain, bursitis or arthritis.

Toe Pain
Common toe pain causes include:
- Gout: This painful “disease of kings” involves build-ups of uric acid crystals in toe joints. If you have gout, you likely experience swelled, painful toes, especially your big toe. As a form of arthritis, gout treatment involves ice packs, NSAIDs, dietary changes and corticosteroids for intense pain.
- Bunions: Although bunions look like growths beside your big toe, they are actually dislocated big toe joints. Pointy-toed shoes can significantly contribute to bunion formation. As with any dislocation, bunions can cause significant pain. Bunion treatment involves comfortable shoes that fit, shoe inserts or surgery for persistent pain.
- Hammertoes: Hammertoes are related to bunions as they are dislocated toe joints in the middle toes. They cause the toes to bend at the joint with a hammer-like appearance. Ill-fitting shoes or muscle imbalances in your feet are common causes. To treat hammertoes, doctors recommend wearing broad-toed footwear and exercises to strengthen and stretch your toe muscles. If the pain does not subside, surgery is an option.
Some other reasons for toe pain may be ingrown toenails, toe fracture or corns and calluses.
Other Causes of Foot Pain
Some of the other reasons your feet can become painful include the following.
Diabetic Neuropathy
Diabetic neuropathy is nerve damage caused by type 1 or type 2 diabetes. Although you can experience diabetic neuropathy in several areas, it often manifests in your legs and feet. Symptoms include sharp pains and tingling or burning sensations occurring anywhere in your feet. Diabetic neuropathy has no cure, so treatment involves a long-term management plan. These plans aim to slow the progression, relieve pain, manage complications and restore function.
Arthritis
Arthritis is not unique to the feet, but it often shows up there. Treatment depends on the arthritis type and also involves a chronic pain management plan. Several types of arthritis can afflict the feet:
- Osteoarthritis, which is cartilage degeneration between your joints and bones.
- Rheumatoid arthritis, an autoimmune disorder where your immune system attacks your joint fluid.
- Psoriatic arthritis, which causes rashes and stiff joints.
Athlete’s Foot
Athlete’s foot is a fungal infection that usually affects the skin between your toes. However, it can spread elsewhere in advanced cases. It involves painful and itchy rashes that can blister. You might experience athlete’s foot when wearing wet or sweaty socks without changing them or going barefoot in public spaces like swimming pools. Treatment involves antifungal cream and powders, but you may need to see a foot care specialist if symptoms do not improve.
Symptoms That Warrant Medical Attention
You can experience foot pain from something as simple as standing on your feet for too long or something as serious as a fractured heel. As such, you may not know if your foot pain is serious enough to see a doctor or if it will improve with rest. To help you know if you should seek medical attention for foot pain, here are some signs that you should see your doctor about your symptoms:
- Chronic pain or swelling in your feet
- Difficulty or inability to bear weight on your feet or walk
- Frequent numbness or tingling sensations
- Infections in your feet
- Intense foot pain
- Open wounds that resist healing
- Tender and warm areas of your feet, especially if a fever is present

See an OIP Orthopedic Doctor About Your Foot Pain
Our board-certified orthopedic doctors and podiatrists at the Orthopedic Institute of Pennsylvania can accurately diagnose the source of your foot pain and provide the most effective treatment option so you can trust the support your feet give you once again. If you are experiencing foot pain and need medical attention, we welcome you to request an appointment to see one of our foot doctors!
Orthopedic Institute of Pennsylvania Opens New Hershey Facility
The Orthopedic Institute of Pennsylvania (OIP) is pleased to announce the opening of its new Hershey facility, offering neighbors in and around the area increased access to orthopedic specialists and services, including general orthopedic care, pain management, podiatry, rheumatology and physical therapy.
OIP has had a presence in Hershey for more than 20 years. This newly renovated, 28,000 square-foot facility, located at 112 Sipe Avenue in Hummelstown, will replace the group’s previous location at 32 Northeast Drive.

Formerly home to the American Cancer Society, OIP purchased the Sipe Avenue property in December 2020 and has spent the last year making extensive renovations to accommodate a full-range of orthopedic services, including on-site physical therapy.
“We are thrilled to expand our presence in the growing Hershey region,” says Will Thompson, OIP’s CEO. “This highly visible office will provide patients in and around the region a convenient orthopedic solution, close to home – and access to a broader range of specialists and services.”
The group officially moved into the new location this month. Currently, six OIP physicians are available for appointments in Hershey with three more expected to join the office this Spring.
The following physicians are currently available for appointments in Hershey:
Patients from the Hershey area, and surrounding communities of Palmyra, Hummelstown, Lebanon, Middletown, Annville, Elizabethtown, Mechanicsburg and more, can find expert orthopedic care minutes from home.
OIP has eight locations throughout the central Pennsylvania area, including Camp Hill, Carlisle, Harrisburg, Hershey, Newport and Millersburg. To schedule an appointment at any OIP office, please call (717) 761-5530 or visit www.OIP.com. For 24/7 urgent orthopedic advice and care, call (855) OUCH-OIP.